
Vaccine hesitancy is so common in Texas that even the youngest clinicians have experience with it. Stephen Line, DO, a first-year family medicine resident at Dell Medical School at The University of Texas at Austin, says it came up with patients he saw in medical school, and now he regularly hears myths and misinformation from patients who don’t trust vaccines.
“Vaccine skeptics are taking their advice from Dr. Google, celebrity blogs, and hearsay,” he said. “It’s very hard to correct that once it’s out there.”
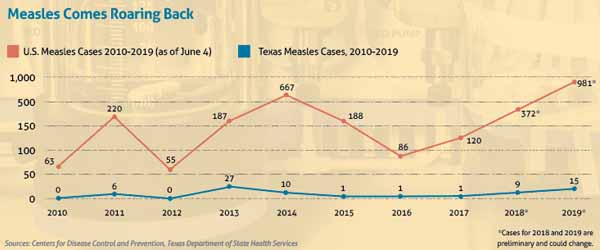
So hard, in fact, that measles – a deadly disease the U.S. Centers for Disease Control and Prevention (CDC) declared eradicated in America in 2000 – has made an unwelcome return in 2019. (See “Measles Comes Roaring Back,” below.)
The reason is twofold, says Trish Perl, MD, chief of the infectious diseases division at UT Southwestern Medical Center in Dallas. First, there’s been a worldwide resurgence in measles, with serious outbreaks in countries like Israel, the Philippines, and Ukraine. Second, Americans who delay or reject vaccinations tend to live or work near each other, and their numbers are growing. When unvaccinated travelers bring measles back to these communities, the highly contagious illness spreads swiftly.
“Once you get a measles case in a community then you can have person-to-person transmission because measles is so infectious and one of the most communicable diseases that exists,” she said. “For every person with measles, it can cause up to 19 cases of measles in a non-immune population.”
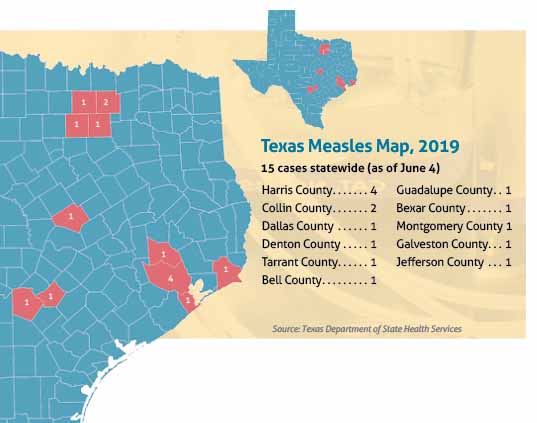
Measles has not spread that fast in Texas – yet. Of the 11 counties reporting cases as of May this year, Harris and Collin counties had the most cases with four and two, respectively. The other nine affected counties all had one case because the immunity conveyed by widespread vaccination has kept the disease from spreading, says Jennifer Shuford, MD, infectious disease medical officer for the Texas Department of State Health Services (DSHS).
However, New York, California, Michigan, New Jersey, Georgia, and Maryland have seen genuine measles outbreaks, which CDC defines as three or more related cases.
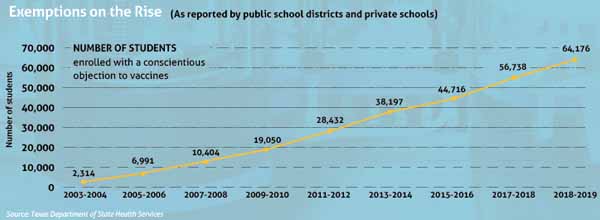
The anti-vaccine movement is weakening Texas’ ability to withstand outbreaks, public health experts say. The number of Texas children exempted from vaccination for non-medical reasons jumped 13% in 2018-19, which doesn't take into account factors such as population growth and school survey participation, according to DSHS. Since 2003, when Texas began allowing parents to refuse vaccinations for reasons of conscience, exemptions have soared more than 2,000% to 64,176 statewide. (See “Exemptions on the Rise,” page 26.)
In fact, three Texas counties – Harris, Tarrant, and Travis – were ranked in the top 25 counties nationwide considered most likely to see a measles outbreak by a May 2019 study done by The University of Texas at Austin and Johns Hopkins University.
Texas Medical Association policy supports medical exemptions from immunizations, but calls for ending all conscientious exemptions “because of the impact on public health.”
Texas will almost surely see a jump in measles cases in coming years, says Peter Hotez, MD, a professor of pediatrics and dean of the National School for Tropical Medicine at Baylor College of Medicine in Houston. California eliminated non-medical exemptions for vaccines in 2016 in reaction to a severe measles outbreak, making Texas the largest state that allows such exceptions, he says.
“Texas is now ground zero of the anti-vaccine movement,” he said.
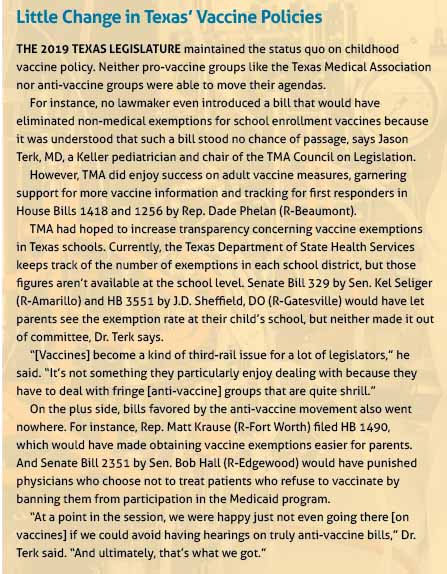
Unfortunately, 2019 ended in a legislative standoff when it came to vaccines, says Jason Terk, MD, a Keller pediatrician and chair of the TMA’s Council on Legislation. (See “Little Change in Texas’ Vaccine Policies,” page 27.) Despite TMA’s lobbying and education efforts like Be Wise – ImmunizeSM, there seems to be little political will at the state and national levels to improve vaccination rates, he says.
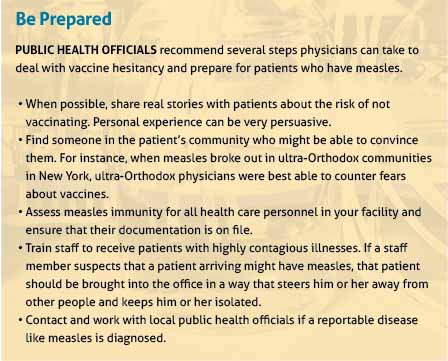
Fortunately, there are still many ways Texas physicians can work with their patients and their communities to educate people and improve vaccination rates, says Wendy Chung, MD, chief epidemiologist for Dallas County Health and Human Services. (See “Be Prepared,” page 28.)
“Knowing what you as an individual physician can do is really important,” she said.
Responding to skeptics
Vaccine skepticism was proudly on display in May at the Texas Capitol in Austin. Texans for Vaccine Choice – the state’s most-prominent anti-vaccine group – held a press conference in one of the building’s large meeting halls.
Two state legislators – Reps. Briscoe Cain (R-Houston) and Bill Zedler (R-Arlington) – attended along with some legislative staffers. The headline speaker was Robert F. Kennedy Jr., son of the late 1968 Democratic presidential candidate.
Mr. Kennedy, a long-time vaccine critic, wound up an almost hour-long PowerPoint presentation by describing a vast pro-vaccine conspiracy against America’s health. He asserted that pharmaceutical companies deliberately use vaccines to make people sick with life-long conditions like autism, depression, and food allergies so that they will become dependent on other drugs; the CDC is essentially a vaccine company; Congress’ oversight of vaccines has been subverted by pharmaceutical lobbyists; regulatory agencies are “sock puppets”; the press has been bribed into silence by advertising; the courts, lawyers, and physicians also have all been bribed or regulated into submission.
“The last thing left is the mom,” Mr. Kennedy told an audience made up mostly of several dozen women and their children. “That’s what all these laws [requiring vaccines] are about is to try to get the mom out of the way.”
The presentation received a standing ovation.
Talk like that frustrates Dr. Hotez but doesn’t surprise him. He has been an outspoken advocate for vaccines, and he wrote the 2018 book about his own daughter Vaccines Did Not Cause Rachel’s Autism to rebut anti-vaccine arguments that vaccines harm people’s health. (See “An In-Your-Face Confrontation with the Anti-Vaccine Movement,” March 2019 Texas Medicine, pages 44-45, www.texmed.org/InYourFace.)
Anti-vaccine arguments, like the autism accusation, typically crumble under even the gentlest scientific scrutiny, Dr. Hotez says.
“We know that autism begins in early pregnancy, long before kids ever see vaccines,” he said.
However, the anti-vaccine arguments are repeated aggressively on a growing network of about 500 websites, Dr. Hotez says. And, he added, anti-vaccine groups change the nature of their rhetoric to suit the local political climate. In Texas, anti-vaccine advocates tailor their appeal to conservative Republicans who dominate the Texas Legislature and statewide offices.
“But they’ll go to the Pacific Northwest and use language that appeals to the far left of the Democratic Party,” he said. “I like to say the one thing uniting the country is the anti-vaccine movement.”
Texas stands as one of 16 states that permits non-medical exemptions from vaccines in schools based on philosophical differences. The meteoric rise in those conscientious exemptions means the state soon will see much higher measles rates unless the 2003 state law is reversed, Dr. Hotez says.
The current national outbreak of measles shows what broad exemptions can do to public health, Dr. Chung says. Because measles is so contagious, it serves as an early warning for other disease outbreaks.
“Any time there’s an increase in vaccine exemptions due to personal beliefs this becomes a tremendous concern because there’s growing potential for a resurgence of these vaccine-preventable diseases,” she said.
In 2014, a measles outbreak involving 147 patients that started at Disneyland in California prompted that state to finally end non-medical exemptions. Something similarly drastic may need to take place before Texas follows California’s lead, Dr. Terk says.
“I regret being pessimistic about the situation, but ultimately I don’t think we’re going to see significant changes in the direction on vaccine policy until we start seeing real-time, real-world consequences – more so than we’ve already seen,” he said.
Containing a killer
At press time, Dallas County had just one of Texas’ 15 confirmed measles cases in 2019. But the story of that one case helps explain how the resurgence of measles consumes time and money for the public, physicians, and patients, Dr. Chung says.
The case started like this: A person who lives in an adjacent county but works in Dallas County traveled overseas and returned home with measles, Dr. Chung says. That one person exposed 90 people in Dallas County to the illness. Of those, 50 people had to have blood drawn to check their immunity status. Twelve were found to be non-immune and quarantined for 21 days. One of them came down with measles – the confirmed Dallas County case.
In communities with low vaccination rates, the investigative work by public health authorities multiplies, as it did in New York City, says Dr. Perl, the UT Southwestern infectious disease division chief. Measles there caused large outbreaks in two communities of ultra-Orthodox Jewish people. Most ultra-Orthodox leaders encourage vaccination, but some people in those two communities believed incorrectly that vaccines violated Jewish religious laws.
Texas public health officials say they cannot yet put a price tag on their efforts to identify and monitor measles patients. But a recent outbreak involving 71 confirmed cases in Clark County, Washington, cost $864,679, mostly to pay for the more than 19,000 hours that responders worked to contain the illness, according to a county news release.
Medical experts say herd immunity for measles breaks down if up to 5% to 7% of children in a community don’t receive two doses of the measles, mumps, and rubella (MMR) vaccine. Currently, state law requires students in kindergarten through grade 12 to receive the MMR shot. Exemptions account for only 1.2 percent of students statewide in surveyed K-12 schools, but exempt students tend to be found in clusters, and that concerns public health officials.
For instance, Texas already has 69 accredited private K-12 schools with vaccination exemption rates in double digits, according to DSHS. Those hotspots include the Austin Waldorf School with a state-high exemption rate of 46%; the Ambleside School of Fredericksburg is second at 35%; and Montgomery County north of Houston has five private schools with exemption rates of 10% or higher.
Unfortunately, exemption rates for public schools are reported only at the district level, making it difficult to tell which specific schools have high exemption rates, says Umair Shah, MD, executive director for Harris County Public Health.
“You may not be aware that where you’re dropping your child off, the specific exemption rate for the school is markedly higher [than the rate for the school district],” he said.
Among Texas’ public universities, state law requires only the meningococcal vaccine for most students to be admitted. Texas Tech University in Lubbock still requires all students to prove MMR vaccination, but most Texas universities do not.
Some, like UT Austin, dropped their MMR requirement years ago, says Melinda McMichael, MD, interim executive director of University Health Services. It seemed extraneous – after all, measles had been declared eradicated, she says.
Texas universities may reconsider requiring the MMR vaccine given the measles resurgence, Dr. McMichael says. But she did not indicate whether UT would be among them.
Improved vaccination is needed at all levels of education, Dr. Shah says. He noted that nearly 300 students and staff at two California universities were placed under quarantine in April after measles outbreaks.
“You don’t want to let your foot off the gas pedal, whether it’s in higher education, or K through 12, or in pre-K,” he said.
Doctors get involved
While vaccine policy changes at the state level may be stalled, public health leaders say physicians can have a direct impact on vaccination policies in local K-12 private schools and day care facilities.
Dr. Chung points out that about 30 Dallas-area Catholic schools uniformly adopted a policy of not admitting students with non-medical vaccine exemptions. Physicians can work with other private schools to reduce or eliminate exemptions.
“We’re seeing a growing number of schools wanting to adopt these policies,” Dr. Chung said. “Parents who are physicians, or who are affiliated with these schools on health boards and advisory committees, are being asked to support the schools in the adoption of these policies.”
Public health officials say family practice physicians and pediatricians who regularly administer vaccines also can look at ways to improve their approach to parents who are vaccine hesitant. For example, Dr. Line, the Dell Medical School resident, says he’s found that a technique called “motivational interviewing” keeps the conversation going when patients try to shut down talk about vaccines. (See Commentary, page 4.)
“One of the things I try to appeal to is that it’s not just about them,” he said. “It’s about the people they’re around and minimizing the exposure they can have [to a preventable illness].”
News of the current measles surge has made Texas physicians more vigilant about vaccine-preventable diseases, Dr. Chung says.
Most of all, Texas physicians must join the ongoing discussion about vaccines, Dr. Shah says. They should engage patient concerns, speak up when fears are expressed in the community, correct misunderstandings, and make it clear that vaccines save lives.
“The vast majority of Texans believe in vaccines,” Dr. Shah said. (See Pulse, page 10.) “However, we cannot be the silent majority. We have to be actively engaged.”
Correction: This story has been edited to say the number of Texas children exempted from vaccination for non-medical reasons jumped 13% in 2018-19.
Tex Med. 2019;115(7):22-29
July 2019 Texas Medicine Contents
Texas Medicine Main
Page