
If you end up among the physicians covered in a wide-ranging quality program launched by Blue Cross Blue Shield of Texas (BCBSTX), you’ll get to see your score for the first time next month.
What’s that score going to look like? No matter how good you feel about your adherence to quality measures, it’s hard to entirely know, because at press time, BCBSTX hadn’t released enough tangible information on one of the three legs of its Physician Efficiency, Appropriateness, and Quality (PEAQ) program – namely, the “appropriateness” part.
Speaking of appropriateness, will your score – which will come from past data that includes 2020 – have appropriate adjustments for the difficulties physicians have faced during the COVID-19 pandemic? Again, unknown.
If you see an error or have a bone to pick with your final PEAQ score, you’ll have 45 days from its online release to make an inquiry – and potentially pursue an appeal – before your score is available to the public. Once you do so, how will that process go? That’s largely another unknown.
In fact, appealing or correcting your score is a part Texas Medical Association physician leaders have particular concerns about as BCBSTX prepares to release PEAQ scores in mid-July. Scores will be released on the online portal Availity, and physicians will get an email notification when they’re available. Then, the 45-day window begins for physicians to make sense of what they see, make sure it looks accurate and representative of their quality performance, and potentially act if it doesn’t.
PEAQ officially launched in January 2020, and TMA, which met with BCBSTX in March about the program, continues to learn about its scoring and administrative aspects.
“In the end, [BCBSTX’] goal is to publicize this data to their members to try to steer them to the most well-behaved doctor in terms of efficiency and quality, to try to drive those goals,” said Amarillo family physician Rodney Young, MD, chair of TMA’s Council on Socioeconomics. “But there have to be winners and losers in a scenario like that. That’s a little problematic. Hopefully it drives all of us toward behaviors that do help to control costs and produce good outcomes. That’s the benefit we hope to realize. But the challenge is in the logistics, the measurement, the delivery.”
What they’re measuring (in part)
BCBSTX declined Texas Medicine’s interview request for this story. At this writing, BCBS had revealed components of only two of the three pieces of PEAQ: efficiency and quality. Appropriateness measures, its December 2019 methodology document said, would be coming “at a later date.”
The methodology doesn’t contain specifics about which physicians are covered in PEAQ and who’s exempt. It said “included specialties” would be released soon, and that some doctors may not be evaluated in the program “for a variety of reasons,” including low volume, a limited number of quality measures, and specialties not being included in the methodology.
San Antonio rheumatologist Chelsea Clinton, MD, chair of the Texas Medical Association’s Council on Health Care Quality, attended the March meeting with TMA leadership and staff. There, she said, BCBSTX indicated it planned to release the first scores on July 15, saying they will be based on 2018-20 data depending on the category. The health plan didn’t give TMA an indication on what if any adjustments would be made for the pandemic, something TMA believes is essential.
“Physicians may have ordered more imaging or lab studies to rule out pathology in patients who wanted to avoid coming to the clinic,” Dr. Clinton said. “For some patients, physicians may have ordered fewer studies in order to protect them from having potentially more exposure to SARS-CoV-2. Patients also often delayed their medical care during 2020 due to the pandemic.”
For the efficiency piece – translation, productivity related to cost – the document said its program would compare physicians with their “peers within the same working specialty and geographic market,” and would compare physicians’ patients with similar patients with similar stages of disease. BCBS is evaluating “episodes of care” for each physician using IBM Watson Health’s Medical Episode Grouper, which it says is used by more than 150 employers, health plans, and state Medicaid agencies.
The quality piece will evaluate physicians based on their performance in an array of metrics, including Health Effectiveness Data and Information Set (HEDIS) measures and how physicians fare in CMS’ Merit-Based Incentive Payment System. (See “Blue Cross’s PEAQ: Measuring Quality and Efficiency,” page 42.)
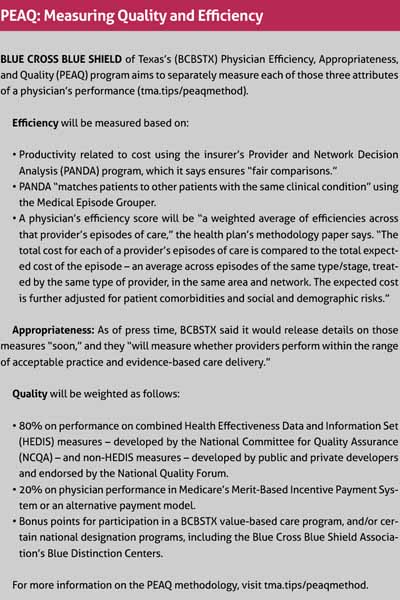
What little information BCBSTX had released on “appropriateness” measurement referred to that category as a solution “to identify and minimize low-value services.” The category will measure whether a physician’s care is following best-practice clinical guidelines, according to BCBSTX’s documents.
To view the methodology document for PEAQ, visit tma.tips/peaqmethod.
Dr. Young referenced an episode of care example BCBSTX used in the meeting he attended: A primary care physician diagnoses a patient with pain in a joint and multiple sites; prescribes Tramadol; refers the patient to a rheumatologist; sees the patient again; and refers the patient to an orthopaedist, who performs surgery.
“That whole thing is one episode of care,” Dr. Young said. “And then if I understood it correctly, the attribution for expense will sort of be based on the whole process. Let’s say for example, I send them to an in-network surgeon, and for whatever reason, that surgeon costs more. Then my efficiency presumably would score lower, even if the care was appropriate and even though I used a network provider.”
On the other hand, Dr. Young said, BCBSTX is “trying to use benchmarks that are becoming more common in a world of measured quality for medical care. They use HEDIS metrics and National Quality [Forum] standards by specialty. Those contain a wide variety of measures that they can choose from, but they’re trying to choose relatively common things, which, that’s a benefit.”
Pursuing an appeal
It’s unclear how much time a physician will have to complete the entire inquiry process. And as doctors are prohibitively busy people, concerns exist about whether they’ll even look at their score, let alone challenge it before BCBSTX releases it to the entire care-seeking world.
“Normally, interactions with insurance companies are not speedy,” Dr. Clinton said.
That’s on top of what Dr. Young describes as a fairly “exhaustive” appeals process if physicians do take issue with any of the BCBSTX data.
“‘Contact us, tell us your concerns, fill out these forms, send them to us, verify your evidence. We’ll schedule a hearing. … Do this. If you don’t like it, appeal to that.’ I mean, at some point it gets absurd,” he said. “Unless you just have a very large panel of BCBS patients where you really have a lot of skin in the game, there’s no reasonable way physicians can go through every one of their payers’ quality performance programs like this one and try to appeal something that they find to be unjust about it.”
For physicians who take issue with their performance data, the inquiry or reconsideration process is the way to remedy it – before, as BCBSTX puts it, “results are posted on the BCBSTX Provider Finder application or publicly through other wider distribution means such as websites.”
“Providers will be able to submit a response within 45 days of initial notification, and a form will be made available and distributable through a portal,” BCBSTX said in its methodology. “A panel with representatives of medical directors, quality and accreditation specialists, network representatives, and data scientists will review the reconsideration request. The provider will be notified of the response to the reconsideration request prior to public posting on sites. Providers can include supplemental information in their requests for reconsideration, which will be used as part of the review.”
A PowerPoint presentation BCBSTX used during its meeting with TMA presents a physician’s initial contact as an “inquiry,” which the health plan will analyze, follow up on, and ultimately resolve via email. From there, if physicians still have “unresolved concerns,” they can request a reconsideration proceeding hosted by BCBSTX, which will result in a “summary of outcomes.”
That reconsideration process looks onerous to Dr. Young, who believes many physicians simply won’t be able to analyze their score and put together an appeal.
“It is not like doctors are sitting around with spare time to sift through these reports. If you do, [that’s] good; I like to think that we’ll look at them,” he said. “But I wish [BCBSTX] would just send you the report rather than making you jump through the extra hoop of needing to log in to get it. I think that will be a challenge. Because if [BCBSTX’] goal is to change physician behavior, but you have to take steps to go in and find [your report], I think there’s going to be a lot of people that are never going to look because they just don’t have the time.”
Tex Med. 2021;117(6):36-38
June 2021 Texas Medicine Contents
Texas Medicine Main Page