
Frisco pediatrician Seth Kaplan, MD, had some concerns about the federal information blocking regulations ahead of their April 5, 2021, implementation date.
The rules require physicians to provide patients – as well other health care professionals treating them – with prompt access to significant portions of patients’ electronic health information upon request.
Dr. Kaplan worried compliance would come at the cost of patient trust if, for instance, an adolescent requested confidential testing for sexually transmitted infections (STIs), but his or her parents had access to the patient portal where those test results would be made available. He also wondered how the rules would affect patients with divorced parents, who may have different levels of legal access to their children’s medical information.
Logistically, his practice was able to comply with the click of a button. Its electronic health record (EHR) already had a box that, when checked, included the clinical note or lab result at hand in the patient portal in real time.
Over the past year, he’s found his concerns have not been borne out.
“The tricky issues about adolescent confidentiality and divorced parents haven’t really come up yet,” he said.
Instead, the regulations’ benefits have revealed themselves. Now, when he refers a patient to a specialist for a consultation, he can access the consulting physician’s notes immediately and review them with the patient, who also has direct access.
“It’s paid huge dividends already,” he said.
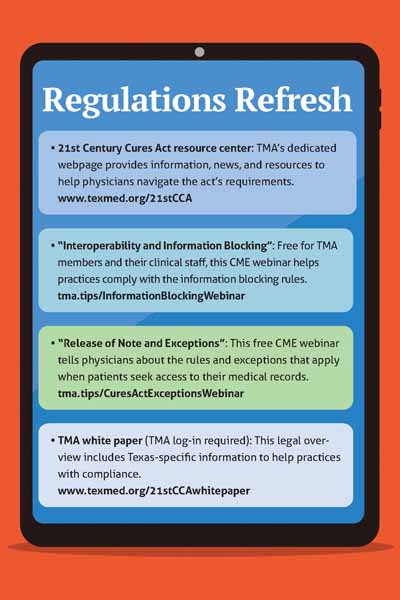
The information blocking regulations stem from the 21st Century Cures Act, which Congress passed in 2016 and federal regulators – namely the U.S. Department of Health and Human Services Office of the National Coordinator for Health IT (ONC) – began implementing in 2020. (See “Regulations Refresh,” this page.)
The types of information within EHRs that physicians must make available are discharge summaries, history and physicals, progress notes, consult notes, imaging reports, laboratory reports, pathology reports, and procedure notes. The law also provides detailed exceptions.
Physicians whose patients request such information must determine the appropriate manner of delivery depending, in part, on the patient’s request and the practice’s technical capabilities. For instance, a patient might ask for access via a patient portal already offered by the practice or a secure email.
In the 14 months since the regulations took effect, some physicians have had their concerns mitigated and their hopes realized. Still, others are wary about the increased administrative burden that comes with compliance and the possibility of violations.
Manish Naik, MD, chief medical information officer at Austin Regional Clinic and a member of the Texas Medical Association’s Committee on Health Information Technology, says these growing pains come with an upside.
“For those who are releasing progress notes or physician notes … the fears about releasing those notes, as expected, haven’t really come to fruition,” he said. “Most of the time the patient actually just has more information to work with, becomes more engaged with their care, and sometimes is more compliant.”
Open-note benefits
Research shows open notes – the automatic release of all clinical notes – generally benefit both physicians and their patients.
In a March 2020 web survey of physicians and other clinicians with a history of sharing notes with patients, 74% agreed it was a good idea, and the same portion viewed it as useful for engaging patients in their care. The JAMA Open Network report also cited previous studies showing patients who were able to access their medical records electronically felt more in control of their care and had a better grip on what their clinician was thinking.
“Open notes may help clinicians, patients, and families improve care by moving toward more open communication and partnership,” the article says.
These findings may assuage physicians on the fence about the information blocking regulations. Compliance also may grow easier as the Cures Act gradually advances interoperability in health care.
The second phase of implementation begins Dec. 31 and requires certified health IT developers to provide upgraded health IT modules that store electronic health information. The final phase starts Dec. 31, 2023, when certified health IT developers must allow for the export of a single patient’s EHR by the patient without assistance and for the bulk export of all patients’ EHRs, which is expected to make it easier for physicians to change EHR vendors. (See “Contract Do’s and Don’ts,” page 28.)
Although Dr. Naik has some reservations about the information blocking regulations, he says improving health IT and EHRs may help ease them.
“With technology … improving, those tools could be used to enhance the way we send results to patients,” he said. That, in turn, could help physicians systematize which information should be released to patients automatically and which qualifies for an exception or should be delayed pending a patient request.
Ongoing challenges
This ramping up may be daunting for physicians who have experienced drawbacks.
Dallas adolescent medicine physician M. Brett Cooper, MD, cites adolescent patient confidentiality and an increased administrative burden chief among his concerns.
In his three-physician practice, he typically meets with adolescent patients alone and then with their parents. If the patient discloses sexual activity, vaping, or marijuana use with the expectation that it is confidential, he must ensure that information is not accidentally released to the parents absent a request from the parents for their child’s medical records. (In such cases, a “preventing harm” exception under the law may allow him to withhold the information.)
Unlike Dr. Kaplan’s EHR, Dr. Cooper’s requires him to uncheck a box to prevent information from being shared automatically to the patient portal. Missing this step could have potentially significant consequences.
“If that note is automatically released to a patient portal without any brokering, I’ve just violated the confidentiality of that patient,” he said, adding that this could cause him to lose his patient’s trust.
Writing two notes – one that can be released to the parents through the patient portal and another that contains sensitive information subject to the preventing harm exception – takes more time.
Dr. Cooper also has received an influx of calls from parents who have gained access to jargon-filled lab results that are harmless and irrelevant to their child’s health but that they want elucidated.
“It’s creating a lot of unnecessary communication,” he said.
In a late 2021 web survey of physicians and other health care professionals, more than 83% reported an increase in patient calls regarding their radiology reports following the removal of an embargo program in anticipation of the information blocking regulations taking effect.
Dr. Naik points out the automatic release of certain information – such as behavioral health clinical notes or pathology results that carry a new cancer diagnosis – could prove harmful to the patient if released without context and create more work for the physician.
“The stress and distress that the patients feel [when they gain access to results] that they don’t understand or are serious could be largely avoided if the doctor had time to explain them to the patient first,” he said.
There are some situations in which a physician can grant a patient’s request to delay the release of their results without the delay constituting information blocking, according to ONC.
For instance, if the physician is performing a sensitive test, such as a biopsy to determine if a tumor is malignant, the patient may request to delay the release of the test results until the physician has reviewed them. In such situations, delays in releasing the results generally should be no longer than necessary to fulfill the patient’s request for physician review.
But, until all EHRs are better able to distinguish between information that should be released to patients automatically and information that requires more physician involvement, Dr. Naik says the regulations’ costs could outweigh their benefits.
The importance of compliance
Despite the issues, it’s critical physicians and other health care professionals comply with the regulations.
ONC received 306 possible claims of information blocking between April 5, 2021, and Feb. 28, 2022. Of those, nearly 80% were filed against physicians and other health care professionals. And nearly two-thirds of the overall claims were filed by patients.
Causing patients to experience unnecessary delays in accessing their electronic health information or charging them to access that information through a patient portal may be considered information blocking.
ONC has not yet released the results of any investigations into these claims or determined the consequences of violating the regulations. Whatever the disincentives, legal and medical practice consultants encourage physicians to get into compliance and to diligently document any exceptions.
Anecdotally, Dr. Naik says patients appreciate the newfound access to their own health information, even if they aren’t yet familiar with the legislation behind the change. He points to the roughly 80% of patients at Austin Regional Clinic who are active users of its patient portal, where electronic health information is shared. After each visit, they also receive a summary, which includes salient points and next steps.
“Patients … tell us over and over again that they really appreciate the fact that we release all that information on the patient portal,” he said. “But I think they [also] appreciate the fact that we interpret those results, so that they can put them into context.”