Castroville family physician Mary Nguyen, MD, estimates she manages half of her patients’ mental health needs.
Her rural, underserved community – about a 30-minute drive from San Antonio – doesn’t have a psychiatrist. The closest one practices in nearby Hondo, but appointment wait times can stretch up to six months, meaning it’s a poor option for patients in distress. Those who can wait often can’t bear the gas costs.
But telehealth has helped Dr. Nguyen meet this need.
For instance, some of her patients with depression are more likely to see her, versus an unfamiliar psychiatrist, for sensitive mental health needs. “It’s easier to be able to talk to somebody who takes care of you for your cough and cold and does your Pap smear,” she said.
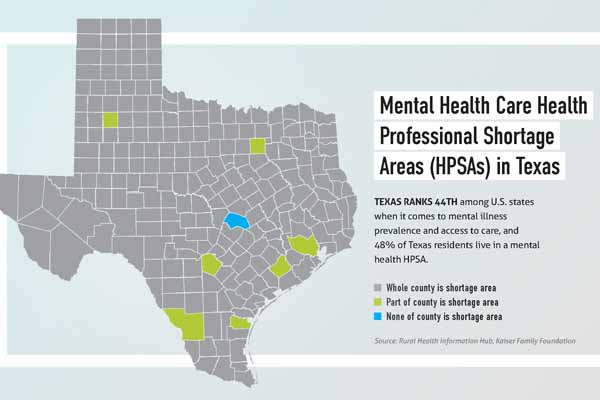
Expanded mental telehealth care is desperately needed to help alleviate the pressure on primary care physicians and expand access for patients amid significant psychiatric workforce shortages. Nearly half of all Texans live in communities with a shortage of mental health care professionals, according to Kaiser Family Foundation. (See “Mental Health Care Health Professional Shortage Areas [HPSAs] in Texas,” page 36.)
In a positive step forward, the Centers for Medicare & Medicaid Services (CMS) recently made permanent certain pandemic-era flexibilities for behavioral telehealth services, namely allowing Medicare patients to access such visits from their homes and via audio-only technology, if they are unable or unwilling to use video. Those changes came after Medicare had moved to permanently cover video-based mental health visits for patients at rural and federally qualified health centers.
These policy updates have proven crucial to Dr. Nguyen’s small, two-physician practice.
“It’s been extremely helpful managing patient care, especially with all the hardships that everybody’s suffered in the past couple of years,” she said.
Under the audio-only provision, her older patients can continue to use a landline for telehealth appointments, which many prefer to the smartphone they either can’t afford or don’t know how to use. It also helps preserve access to mental health care in rural areas plagued by shoddy broadband access. During the early months of the pandemic, she says some patients would attend telehealth appointments from her office parking lot, where they could siphon the necessary Wi-Fi, which was unavailable at home.
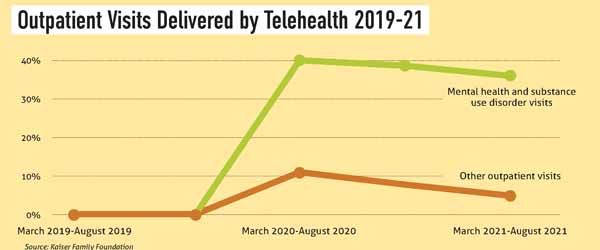
The COVID-19 pandemic catalyzed the widespread use of telehealth as well as the regulatory changes that made it possible. Behavioral health – which includes mental health and substance use disorders – was particularly well suited for this modality, given that patients don’t need to be seen in person to reap the benefits of treatment and that demand far outweighs supply, according to the American Telemedicine Association. Research also shows behavioral telehealth visits rose faster – and remain more common – than other virtual visits over the course of the pandemic. (See “Outpatient Visits Delivered by Telehealth 2019-21,” below.)
Texas physicians say behavioral telehealth regulatory changes have already proven beneficial – and could be maximized with additional policy reforms, like payment parity for all telehealth visits. In the meantime, the gains of the past few years have forged a path toward future telehealth expansion beyond behavioral health.
The Texas Medical Association and the American Medical Association continue to urge federal lawmakers to make permanent Medicare’s telehealth payment and regulatory flexibilities for all specialties.
Stretching a thin workforce
Fort Worth child and adolescent psychiatrist Debra Atkisson, MD, has seen behavioral telehealth expand access to care for her young patients impacted by serious psychiatric workforce shortages, as well as for rural and older patients.
“By continuing to use telepsychiatry and continuing to keep some of the types of obstacles waived [like site restrictions and video capability requirements], we’re able to get better access for people, better compliance, and good outcomes for patients,” she said.
Anecdotally, she notes behavioral telehealth care incentivizes compliance among patients, who appreciate the convenience and are less likely to miss virtual appointments than in-person ones.
Austin family physician Kevin Spencer, MD, turns to the Austin-based behavioral telehealth company Televero Health, which serves primary and specialty care groups – like Premier Family Physicians, where Dr. Spencer is the CEO and president – that refer patients with acute and moderate needs.
TMA continues to advocate that lawmakers, regulators, and payers don’t unfairly favor telemedicine-only companies, while recognizing such innovations can help fill gaps.
Dr. Spencer says Premier Family Physicians started using Televero in October 2020 after years of struggling to find psychiatrists and therapists who would see patients promptly and accept insurance. Today, Premier’s roughly 30 physicians refer about 75 patients to Televero each month for psychiatric and counseling services.
“We went from not having a good psychiatric referrals base that was consistent … to now we can get our patients seen very quickly,” he said.
Dr. Spencer acknowledges the concerns about high-volume telehealth companies. But he touts Televero’s model, which he says centers a close relationship with the referring primary care physician.
“While it’s online, it’s people with Texas licenses who understand our community [and its resources],” he said.
Ray Wolf, Televero’s chief operating officer, says the new behavioral telehealth flexibilities have made it easier for patients to follow through on their physicians’ referrals. For instance, Televero reports that 10% to 15% of its appointments are conducted via audio-only technology, which allows patients to keep their appointments, even if they aren’t tech-savvy or they’re dealing with intermittently spotty internet service.
“Every little bit of friction, you have to keep taking out of the system,” he said.
On the physician front, Dr. Atkisson adds that behavioral telehealth enables more flexible work schedules that in turn, can help with employee retention. Three years into the pandemic, such flexibility is paramount to an overworked and burnt-out health care workforce. (See “Wellness First,” page 12.)
“It’s still a huge issue that we have a lot of people in the medical field, but especially in mental health, who are really looking at, ‘Do I need to work part-time for a while? Do I need to retire? Or can I work longer due to the convenience of telepsychiatry?’” she told Texas Medicine.
And Medicare’s policy changes have served as a bellwether, spurring private payers to follow suit.
“In the private insurance world, what I have been seeing is that they have been honoring those same guidelines as what CMS has put forward,” Dr. Atkisson said. “The lens through which we’re looking at the treatment of patients is that the increase in telepsychiatry is going to continue.”
Caring for the whole patient
As a family physician who cares for the whole patient, Dr. Nguyen does want to see the government make permanent telehealth flexibilities for all specialties.
“It doesn’t make sense to carve out mental and behavioral health and not encompass all the components of a patient’s health,” she said, adding that mental illness often manifests as physical symptoms, such as a chronic sore throat or fatigue, that physicians also must treat.
TMA and AMA continue to monitor federal and state efforts that appear to be moving in that direction.
Congress voted in March to extend Medicare’s telehealth flexibilities – including waiving site restrictions and allowing audio-only for physical health visits – for five months after the COVID-19 public health emergency ends. More recently, the U.S. House in August overwhelmingly passed the Advancing Telehealth Beyond COVID-19 Act, which would extend Medicare’s pandemic-era telehealth policy changes across all specialties through the end of 2024. The bill is now in the hands of the U.S. Senate.
However, some federal lawmakers are wary of extending these changes beyond behavioral telehealth care, citing the potential for patient overuse, fraud, and abuse, according to an April 2022 report by the Committee for a Responsible Federal Budget.
Austin psychiatrist Thomas Kim, MD, a consultant to TMA’s Committee on Health Information Technology, acknowledges these concerns but says there are safeguards in place – such as medical claims review – to address them.
He also stresses the benefits of telehealth for other specialties versus what he describes as “arbitrary limitations” to behavioral health. For instance, surgeons can use telehealth to conduct post-operative visits where appropriate, saving patients time and discomfort during the recovery period.
“It just makes sense [to extend these flexibilities to all specialties] when you talk about an environment of limited resources,” he said. “There’s a reason why the word ‘crisis’ is being bandied about, whether it’s mental health [care] or health care in general.”
Dr. Kim also hopes the Texas Legislature will build on recent TMA-backed telehealth wins – including 2021 laws that expanded telehealth payment in Medicaid and created a state broadband office – by prioritizing payment parity during the upcoming session, which begins in January.
The Texas House Committee on Public Health in September began deliberating its interim charges to address Texas’ health care workforce woes, during which TMA advocated physicians should be paid the same rates and held to the same documentation and medical record retention standards for telehealth visits as they are for in-person visits. TMA also asked committee members to prevent state health plans from unfairly favoring telehealth-only companies, such as by waiving copays.
Without these steps, TMA said in written testimony, physician practices may no longer be able to provide telehealth services, leaving patients in the lurch.
“Today, more patients have experienced the convenience of telemedicine and want to continue receiving care this way.”