
The rise of telemedicine during the COVID-19 pandemic has spurred a change in state law that will not only help make certain telemedicine services permanent but also give out-of-state physicians an easier pathway to join the Texas workforce.
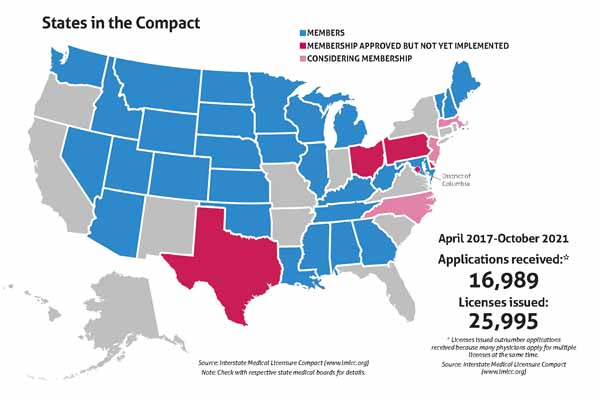
Thanks to the 2021 Texas Legislature’s regular session approval of House Bill 1616 – authored by Rep. Greg Bonnen, MD (R-Friendswood), in the House and sponsored by Sen. Joan Huffman (R-Houston) in the Senate – Texas will join the Interstate Medical Licensure Compact. That agreement, which the Texas Medical Association has supported, simplifies the process for highly qualified physicians licensed in other states to be licensed in Texas.
The agreement also will let Texas physicians more easily obtain medical licenses in the 29 states that are currently members of the compact along with Guam.
“The pandemic opened up opportunities to deliver telemedicine because numerous state and federal waivers allowed physicians to deliver safe care even in the absence of full licensure in other states. But as the pandemic winds down, as the public health emergency waivers are rescinded, it’s especially important that physicians are able to obtain multistate licensure. And the compact is an opportunity to do that,” said Welela Tereffe, MD, a radiation oncologist and chief medical executive at The University of Texas MD Anderson Cancer Center in Houston.
The compact also comes at a time when Texas continues to do an excellent job of attracting new physicians, with newly licensed physicians hitting another all-time high. In fact, recent data show physician growth is finally outstripping population growth. (See “Texas Keeps Attracting New Physicians,” page 40.) Texas issued 813 emergency medical licenses during fiscal year 2021, according to state data, 41% of which were for physicians associated with a telemedicine company.
Recruiting for Texas
TMA had pushed for Texas to join the interstate compact in previous legislative sessions, but the emergence of telemedicine during the pandemic finally made the case irresistible for lawmakers in this year’s regular session, says Dan Finch, TMA vice president for advocacy.
About 80% of U.S. physicians meet the criteria for a license through the compact, according to the compact’s website. Out-of-state physicians will be able to obtain a Texas medical license more quickly, allowing physicians to move to Texas and begin helping patients quickly, Dr. Tereffe says.
“That’s going to make Texas a more attractive place for physicians to relocate to and allow Texas hospitals to recruit the very best physicians from around the country,” she said, adding it will also make it easier for out-of-state physicians to practice telemedicine in Texas.
That, in turn, could help Texas with its chronic shortage of physicians, Mr. Finch says.
For instance, 32 of Texas’ 254 counties have no primary care physician, and the shortage is even more severe in certain specialties, according to the Texas Department of State Health Services (tma.tips/DSHSHealthProfessions). In 2020, 170 counties had no psychiatrist.
As for getting licensed in other states, Texas physicians already can do that, but the process typically takes up to a year, Mr. Finch says. The compact will speed up that process to about five or six weeks for physicians who qualify.
“It just makes getting a license in another state breathtakingly simple,” he said. “This is only going to help Texas physicians.”
Telemedicine’s role
Telemedicine also highlighted the need for out-of-state licensure for large medical institutions like MD Anderson that treat numerous patients from other states, Dr. Tereffe says.
“We had a limited range of virtual care options available, but when the pandemic hit, it really accelerated our efforts,” she said. “And we have conducted close to 300,000 virtual encounters since the start of the pandemic. Many institutions around the country saw their percentage of visits through telemedicine zoom up to even the 90% range in the early months of the pandemic, March to July of 2020. A lot of institutions have seen those numbers go down to the single digits. What we saw was that about 30% of visits were converted to telemedicine in the early days of the pandemic, and they’re now holding steady at about 20% to 25%.”
At the same time, about 25% of MD Anderson patients come from out of state for cancer treatment, Dr. Tereffe says. Frequently, that involves surgery, and the post-surgery recovery can last days or weeks.
“When they’re discharged, they want to go back home because they recover best in the environment where it’s most comfortable for them,” she said. “But they also need to have routine check-ins with their physician to make sure that their wound is healing well, to make sure that they’re resuming routine activity, to address any pain issues that might be coming up. So that’s always been very challenging for those patients. Do they stay in Houston weeks just so they can visit with their physician on a periodic basis? It’s very expensive and very dislocating.”
With the increased use of telemedicine during the pandemic, a growing number of patients now expect to return to their home state and remain under the care of the Texas physicians who treated them, Dr. Tereffe says. Many patients still return to Houston for check-ups or follow-up care. But telemedicine – aided by Texas physicians with out-of-state licenses – can minimize the number of those visits.
“It’s a huge benefit for continuity of care for patients who come to us from outside the state of Texas,” she said. “They can use a mixture of virtual and in-person visits in a way that keeps them safe and maximizes their outcomes in terms of their cancer treatment and limits the cost that they have to bear.”
The pandemic also has increased the need for remote patient monitoring – using devices and apps to monitor a patient’s health from a distance, Dr. Tereffe says. (See “Accelerating RPM,” March 2021 Texas Medicine, pages 40-43, www.texmed.org/ AccelerateRPM.) Licensure through the compact will help physicians who have patients who need that service when they cross state lines.
“We can allow those patients to return home and then use a variety of remote monitoring and video consultations to check on how they’re doing and make sure they’re recovering well,” she said.
But not all states belong to the compact, Dr. Tereffe says. Physicians participating in the compact will need to be vigilant that they’re not providing care in a state for which they don’t have licensure.
“Physicians should never assume that it’s acceptable to care for their patient who is in another state if they don’t have licensure there,” she said. “They should check the rules of that medical board to make sure they remain in compliance.”
Getting a compact license
Obtaining a medical license through the Interstate Medical Licensure Compact will have no direct impact on a physician who already has a Texas medical license, according to the Texas Medical Board (TMB), which oversees licensing for Texas physicians.
The new license will have the same privileges as the Texas license, but physicians will have to meet all state requirements on licenses they seek through the compact, including CME requirements. Also, a Texas physician with an out-of-state license can face reciprocal disciplinary or remedial actions on all licenses obtained through the compact, TMB says.
The criteria for obtaining a compact license are more stringent than what is needed to obtain an in-state medical license (tma.tips/CompactQualify). Physicians must first establish a “state of principal license,” according to the website for the Interstate Medical Licensure Compact. To do that, physicians must hold a full, unrestricted medical license in a state that is a member of the compact.
In addition, at least one of the requirements below must apply. The physician must have:
- Primary residence in the state of principal license;
- At least 25% of his or her practice in that state;
- An employer who is located in that state; or
- Use that state as state of residence for U.S. federal income tax purposes.
The other criteria focus on safety and ensuring that experienced physicians apply. Physicians must:
- Have graduated from an accredited medical school, or a school listed in the International Medical Education Directory;
- Have successfully completed graduate medical education at institutions accredited by the Accreditation Council for Graduate Medical Education or the American Osteopathic Association (AOA);
- Have passed each component of the United States Medical Licensing Examination, Comprehensive Osteopathic Medical Licensing Examination USA, or equivalent in no more than three attempts for each component;
- Hold a current specialty certification or time-unlimited certification by the American Board of Medical Specialties or the AOA Bureau of Osteopathic Specialists;
- Not have any history of disciplinary actions toward a medical license;
- Not have any criminal history;
- Not have any history of controlled substance actions toward a medical license; and
- Not currently be under investigation.
The process for applying comes in two parts, according to Marschall Smith, executive director of the commission that oversees the compact. The first part is the application, which results in a “letter of qualification” – a vetting of the physician. That can take 30 to 45 days. Once the letter of qualification is completed, obtaining any out-of-state license typically takes seven to 10 days.
“That is why a lot of physicians who are in telemedicine or want to practice in multiple states always keep a letter of qualification active,” Mr. Smith said.
Participating in the compact costs $700 plus the local fees for each license obtained, per the compact’s website.
TMB plans to make Jan. 1, 2022, the first day out-of-state physicians can apply for Texas licenses through the compact and that Texas physicians can apply for out-of-state licenses, according to board spokesperson Jarrett Schneider.
However, TMB and the commission administering the compact are still ironing out technical, financial, and staffing questions, meaning that actually obtaining a license through the compact likely will not be possible until later in 2022.
“The TMB has also been working with the Interstate Medical Licensure Compact Commission on developing processes and procedures for the new licensure pathway,” TMB Executive Director Stephen Brint Carlton said in an email statement.
Although no date for implementation has been set, TMB will continue to update physicians on its website, he says (tma.tips/TMBcompact).
Tex Med. 2021;117(12):38-42
December 2021 Texas Medicine Contents
Texas Medicine Main Page