Editor’s note: This article was submitted by the Office of Inspector General as part of a campaign to help educate physicians and other health care professionals preventively identify and avoid common billing mistakes.
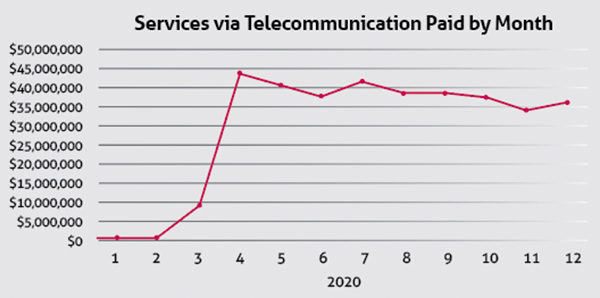
COVID-19 prompted an increased need for telemedicine services to connect physicians with their patients. To quickly meet that need, Texas Medicaid adopted waivers and changed policies to ease technology restrictions and expand the number of Medicaid services available virtually. Reimbursement for telemedicine and telehealth averaged less than $800,000 per month in 2019. By April 2020, Medicaid payment for virtual services jumped to $43 million, and averaged more than $37 million monthly throughout 2020.
The significant shift towards virtual service delivery, especially for services for which telemedicine was not a prior benefit, presented new program integrity challenges for the Texas Health and Human Services (HHS) Office of Inspector General (OIG). With a mission to protect program integrity and ensure patients obtain medically appropriate care, the OIG prevents, detects and deters fraud, waste and abuse in the delivery of Medicaid and CHIP services.
Working with physicians, health care professionals, managed care organizations (MCOs) and other HHS agencies helps the OIG identify risks and collaboratively develop solutions. Over the past year, the office has worked to identify potential improper billing related to COVID-19 with the goal of helping physicians and health care professionals avoid common billing mistakes that could result in recoupment later.
Using terminology set by state law, Texas Medicaid “telemedicine” services are delivered by a physician, or a health professional acting under the direction and supervision of a physician.
“Telehealth” generally refers to a health service other than telemedicine delivered by a licensed or certified health professional, such as registered nurses, occupational therapists, home health agencies, or licensed professional counselors.
MCO payment
Medicaid and CHIP Services advised MCOs that payment for telemedicine services should be medically appropriate, clinically efficacious, and cost effective. Moreover, telemedicine must:
- Be provided in accordance with state and federal law and meet the same standard of care as an in-person health care service; and
- Promote and support patient-centered medical homes.
Potential risk indicators
The examples presented in this article are a result of OIG analysis, stakeholder input, Healthcare Fraud Prevention Partnership information sessions, and collaboration with the National Health Care Anti-Fraud Association.
Multiple services within a brief time
While an increase in overall telemedicine services is expected with the pandemic, certain billing patterns can indicate potential billing errors or even suspicious activity. One issue of interest is billing for multiple telemedicine or telehealth services on the same patient in a short period of time, such as within one month or even within one day. In general, it is not uncommon to see multiple services, such as counseling or therapy sessions, provided via telehealth more than once a month. However, multiple visits in one month via telemedicine to the same health professional may be unusual if they did not occur with that frequency prior to the pandemic.
Examples of potential improper billing include:
- Physicians calling patients as a “follow up” within the same week as a telemedicine visit and billing an Evaluation and Management (E&M) code for that call.
- Physicians performing telemedicine visits, then an in-person visit, with a modifier 25 (separately identifiable service) for the same diagnosis.1
- Physicians calling patients they had not recently seen and who had not requested an appointment to “check up” on them and billing an E&M code.
Impossible hours
Health care professionals billing impossible hours occurred prior to the pandemic for behavioral health, therapy and attendant care services. However, telemedicine services are also vulnerable to the same scenario. Using timed procedure codes, health professionals are flagged in excess of 24 billed hours in one day. There are situations in which telehealth services are billed more than 24 hours by a single provider, due to services being rendered by assistants. If this is the case, it is taken into consideration.
Telephone-only services
Telemedicine provided via telephone–only introduces a new facet in terms of E&M. Billing more than one E&M code a day on a patient, with a modifier 25, would lead to improper reimbursement. The Texas Medical Board and HHS issued guidance regarding billing for telephone calls.234 E&M services cannot be billed if the physician determines an in-person or video telemedicine visit is required within 24 hours of the next available appointment time, as the services rendered via telephone will be considered part of the office/video visit. If a call follows an office visit within seven days for the same diagnosis, the telephone call is considered part of the previous visit and cannot be billed separately.
Documentation requirements
Telemedicine services carry the same recordkeeping and note-taking standards as services performed in person, according to the Texas Medical Board.5 Given the regulation waivers that now allow physicians to establish patient relationships and prescribe controlled substances via telemedicine—including audio-only visits—and get paid at the same rate as in-office visits, physicians must continue to demonstrate that services were provided and met the standard of care.
Services provided via telecommunications are required to be documented completely in parity to in-person visits, including observations, diagnosis, testing, and treatment plan. Patient consent for treatment via a virtual visit also is required.
COVID-19’s evolving impact on health care delivery necessitates physicians’ ongoing attention to remain in compliance. For the latest updates on telemedicine flexibilities, extensions and requirements, physicians are encouraged to visit the Texas HHS website, hhs.texas.gov.
Identifying potential errors and fraud
The OIG will continue to explore current and emerging program integrity risks related to the COVID-19 pandemic. In so doing, the OIG’s goals are to not only identify and stop actual fraud and abuse, but also to better educate physicians and health care professionals about how to avoid unintentional errors that may result in recoupment later. This includes analyzing encounter data and revising algorithms to detect potential improper payments.
The OIG investigates fraud, waste and abuse following referrals from an MCO’s Special Investigative Unit; reports from patients, physicians, or other health professionals to the OIG Fraud Hotline and website; and as a result of the OIG’s data-driven analysis. Based on the findings of a preliminary investigation, a case may be closed; concluded with a recommendation for education; referred to the OIG’s Provider Investigations unit for a full-scale investigation; or referred to another agency or entity, such as the Attorney General’s Medicaid Fraud Control Unit when criminal Medicaid fraud is suspected.
Investigation outcomes may include education, prepayment review of claims, penalties, required repayment of Medicaid overpayments, and/or exclusion from the Medicaid program.
Reporting a problem
Physicians who suspect fraud, waste or abuse by a provider or a patient may report it to their MCO or the OIG via its Fraud Hotline (800-436-6184) or website, ReportTexasFraud.com.
To learn more about the Office of Inspector General:
References:
https://www.tmhp.com/news/2020-03-20-claims-telephone-audio-only-medical-services
https://www.tmb.state.tx.us/idl/53F6A668-7BCF-B0D2-78E3-CCE4C3397F78
https://www.hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2020/sb-789-telemedicine-telehealth-hts-medicaid-dec-2020.pdf
1 TAC §354.1432
https://www.tmb.state.tx.us/idl/53F6A668-7BCF-B0D2-78E3-CCE4C3397F78
Tex Med. 2021;117(9):43-45
September 2021 Texas Medicine Contents
Texas Medicine Main Page