 What areas of Texas are using emergency departments the most? Where are conditions like diabetes, dementia, and chronic obstructive pulmonary disease (COPD) most prevalent? And, what social factors in different corners of the Lone Star State are driving those characteristics and outcomes?
What areas of Texas are using emergency departments the most? Where are conditions like diabetes, dementia, and chronic obstructive pulmonary disease (COPD) most prevalent? And, what social factors in different corners of the Lone Star State are driving those characteristics and outcomes?
After three years of work, the Center for Healthcare Data at McGovern Medical School at UTHealth is sharing part of its growing trove of numbers for data-driven discussions on those and many other aspects of health care in Texas.
The center doesn’t have all the answers. But its work under a federal certification from the Centers for Medicare & Medicaid Services (CMS) has resulted in valuable state and regional statistics that the center leaders believe provide food not only for thought, but also for policy.
About three years ago, UTHealth earned “Qualified Entity” certification from CMS. That gave its Center for Healthcare Data access to a wealth of Medicare claims data that – along with commercial-payer data – can help shine a bright light on what’s going on in Texas health care.
Via the center’s Health of Texas Dashboard, anyone can view and click dozens of stats for 2016, pulled from both government and commercial claims data.
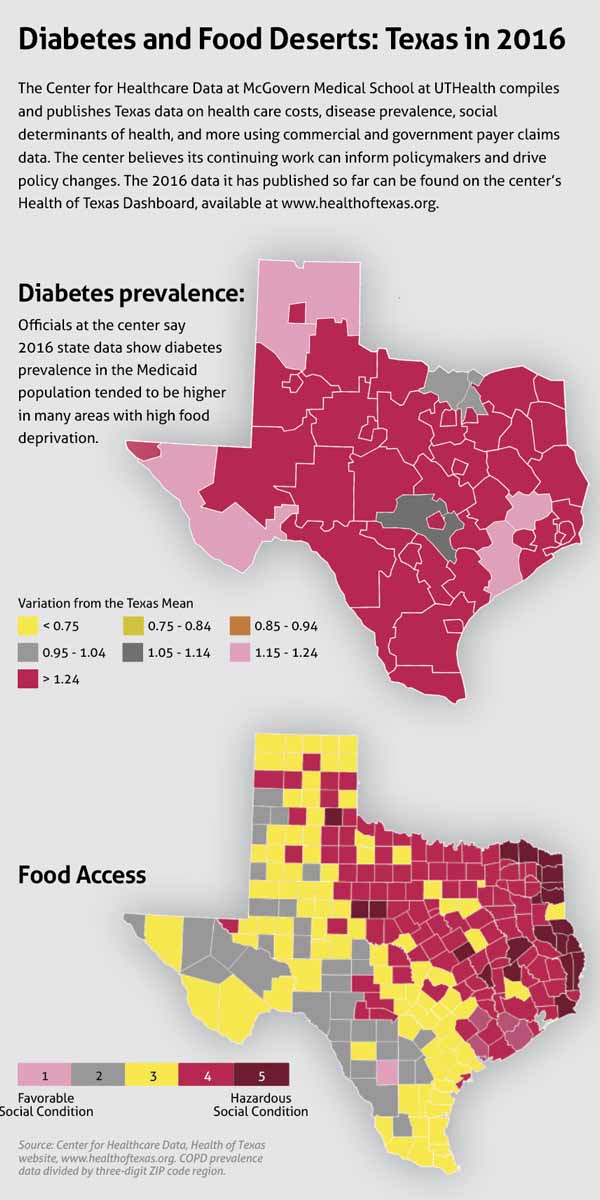
And thanks to input from Texas Medical Association members and others, the website includes an entire section of data on one of the most talked-about topics right now in health policy: social determinants of health. That section highlights county data on food availability, smoking, drinking, and obesity, among other health impacts. (See “Diabetes and Food Deserts,” page 41)
More recent data is on the way. But the 2016 information already available gives everyone from physicians and researchers to lawmakers plenty to click through and digest.
Austin family physician Ajay Gupta, MD, a member of TMA’s Council on Health Care Quality, says there’s tremendous value in the kind of data the center is distributing.
“Anytime you can take claims and learn more about your population in a particular area, you can use that data to help drive [improvement] initiatives,” he said.
What’s there
Receiving certification in CMS’ Qualified Entity program entitles organizations to Medicare Parts A, B, and D claims data “for use in evaluating provider performance.” The organizations that CMS certifies are required to use the data for public, CMS-approved reports. (See “A Wealth of Information,” November 2017 Texas Medicine, pages 47-53, www.texmed.org/wealthofinfo.) As of October 2019, UTHealth is one of 27 qualified entities listed on CMS’ website.
Trudy Krause, PhD, co-director of the center, says it has all 2016 Texas claims data from Medicare and Medicaid. As of mid-March, it was awaiting the go-ahead to publish traditional Medicare data, but Medicare Advantage and Medicare Supplemental data already were available on the website. The Health of Texas Dashboard also includes commercial claims, although some carriers hadn’t given the center permission to use their data, Dr. Krause said.
The center has spent the past couple of years standardizing the data and making it ready for publication.
“With 100% Medicaid, 100% Medicare, and … I think, between 40% and 60% of commercial, it really gives us a pretty good representation [of] the state,” Dr. Krause said. “One of the tabs on the website shows you exactly the percentage [of the population] covered in each of the geographic regions. So it helps researchers see whether it’s an appropriate representation of that region. Because some of the regions may be covered by a single commercial carrier, and it might not be as well-covered as some of the metropolitan areas.”
 Social determinants
Social determinants
The dashboard includes tabs broken down into several categories such as Cost, Utilization, and Prevalence. On most of those tabs the state is grouped by three-digit ZIP code regions.
Click on the Utilization tab, for example, and you’ll see that within the Medicaid population, emergency department (ED) visits are extremely frequent on the eastern border of Texas, compared with the state average.
The decision to include social determinants of health came as a result of TMA recommendations, says Kalyani Sonawane, PhD, assistant professor at the Center for Healthcare Data. She says UTHealth sought feedback not only from TMA, but also from other entities representing likely users of the Health of Texas tools, such as the U.S. Department of Health and Human Services and hospitals in Houston’s Texas Medical Center system.
“In terms of what should be on the dashboard, CMS only requires us to put cost and quality. But we constantly got feedback from clinicians from TMA that social determinants of health are becoming such an important part of the costs of care and how much they affect the outcomes of these patients,” Dr. Sonawane said.
Those social determinants can provide a crucial window into the “why” behind the numbers elsewhere. Cecelia Ganduglia-Cazaban, MD, co-director at the Center for Healthcare Data, says the ability to combine information makes the tool much more powerful than it would be otherwise. For instance, if you use the dashboard to look up COPD prevalence across Texas, you’ll see a large swath of both the north and east areas of the state are in red, or well above the state’s average.
Then, if you scroll over to the Social Determinants of Health tab and look up adult smoking in the general population, those same regions are filled with counties in red and orange – the two colors representing the most “hazardous social conditions” for that measure.
“It was very interesting when we looked at COPD, how clear a pattern it was that it was an issue in eastern Texas across the different payers,” Dr. Ganduglia-Cazaban said.
The data show a high prevalence of food deserts in areas where the prevalence of diabetes is high, Dr. Sonawane adds. Many counties with the state’s highest “hunger scale” sit on Texas’ eastern/northeastern border. Meanwhile, diabetes prevalence is high in the same region among both the Medicaid population and the commercial population.
“We think this has a tremendous value for policymakers and state agencies,” Dr. Ganduglia-Cazaban said. “We hope that it can help inform policy and can help also trigger ideas … for different researchers and organizations across our state to create information that can help drive policy.”
Future data, future impact
Dr. Gupta, the Austin family physician, is the chief medical officer for Health Insurance Marketplace plans in North Carolina and Tennessee. He says those plans use data similar to what UTHealth compiles.
With such information, he says Texas could replicate something like North Carolina’s NCCARE360, a state-funded coordinated care network that uses social determinants of health as part of a system to connect people with the resources they need.
“If you see an area that you may notice has a higher diabetes prevalence, that would help drive initiatives for action towards those areas,” Dr. Gupta said. “So if it’s a mobile food bank, or if it’s [getting] diabetes educators out to that particular area, working with local services to help getting needed supplies or medications to that area, that’s extremely helpful.”
Even after UTHealth’s Center for Healthcare Data publishes all the commercial and government claims data at its disposal, Dr. Ganduglia-Cazaban notes one major population will remain unaccounted for: the uninsured.
“Because we don’t really have data on them. It’s one of those areas that I would really like to incorporate at some point, but it’s not an easy task to get data on them.”
Even so, newer and older data will be coming to the Health of Texas dashboards in the coming months. The center is constantly compiling more metrics as well, Dr. Krause added.
“We wanted to get through the process first, and now that we’ve done that, we can add more and more to the site, and that will be continually happening,” she said. “And we welcome people’s input. If there’s something that an organization feels is important to see, we want to add it.”
Tex Med. 2020;116(5):40-42
May 2020 Texas Medicine Contents
Texas Medicine Main Page