Helping patients who’ve developed workplace illnesses almost never turns out to be simple or straightforward. For Tyler internal medicine specialist Jeffrey Levin, MD, one case several years ago highlighted the many things that can go wrong. It involved a worker at a Texas rock-crushing company.
“[He] first made his way to see me because he had latent tuberculosis, and it turns out that a risk factor he had for tuberculosis was that he had underlying silicosis associated with the rock-crushing operation,” said Dr. Levin, former chair of the department of occupational and environmental medicine at The University of Texas Health Science Center at Tyler (UTHSC-Tyler).
Dr. Levin tried to help the man with his worker’s compensation claim and also recommended restricting his work and dust exposure. The man was fired from his job. When Dr. Levin reached out for assistance to the U.S. Occupational Safety and Health Administration (OSHA) and state agencies, they told him there was nothing they could do. Dr. Levin eventually referred the man to legal help, but the patient never could return to his job and, in time, died due to his illness.
Workplace illnesses can be difficult for physicians and patients because some take years to develop and frequently are masked or mimicked by other illnesses, Dr. Levin says. Such a disease may not show itself until decades after the patient has left the job that caused the problem. By then, the illness may be so far along that little can be done.
That time lag between exposure and illness is just one of several difficulties Texas physicians face in tackling workplace illnesses. Because Texas does not have a federally-approved plan for developing and enforcing workplace health and safety standards, the state defers to OSHA on this responsibility, Dr. Levin says.
OSHA considers an illness work-related “if an event or exposure in the work environment either caused or contributed to the resulting condition or significantly aggravated a pre-existing condition,” according to the U.S. Bureau of Labor Statistics.
OSHA recognizes dozens of work-related illnesses, ranging from heatstroke and contact dermatitis to occupational asthma, but physicians are required to report only four to the Texas Department of State Health Services (DSHS): silicosis, asbestosis, pesticide poisoning, and lead poisoning. (See “Reported Job-Related Illnesses in Texas, 2016,” right.)
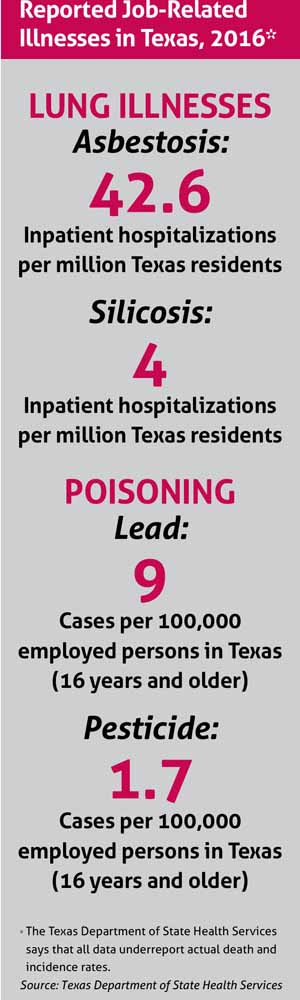
All of these illnesses are underreported, says Ketki Patel, MD, senior epidemiologist at DSHS who oversees the reporting. The problem occurs nationwide, not just in Texas, she says.
Perhaps the biggest reason for underreporting is the delay between exposure and the first symptoms. Even when physicians ask about current occupation, they almost never ask about past jobs that could have a direct bearing on the patient’s health, says Cynthia Ball, DO, chair of the department of occupational and environmental health sciences at UTHSC-Tyler.
“Asbestos and silica are good examples of exposures that may not manifest clinically for years,” she said. “Without pre-visit planning and inclusion of these questions on [patient] forms, a clinician may not have an opportunity to ask when face time [with the patient] is limited to elicit this information.”
Combatting those and other occupational illnesses is just as important for a community’s health as providing vaccines or ensuring clean drinking water.
“Occupational and environmental factors contribute to disease,” Dr. Ball said. “And if you look at the 10 most important public health initiatives of the past century, workplace safety is one of them.”
Significant underreporting
News of underreporting has made occupational illnesses an emerging issue, Dr. Levin says, and silicosis has earned more attention than others in recent years. In 2016, OSHA issued rules designed to protect workers from inhaling silica dust, a problem affecting potentially 2.3 million workers in the U.S. and thousands in Texas, according to the U.S. Bureau of Labor Statistics.
The new rules imposed tighter standards on businesses where silica dust threatens workers’ health, requiring dust suppression with water and better ventilation. In Texas, two of the businesses most directly affected are petroleum fracking companies, which pump tons of silica sand deep into the earth, and companies that cut, grind, and polish “engineered” – or human-made – stone countertops, Dr. Levin says.
Despite the updated regulations, experts in workplace health felt that cases of silicosis were being missed at least in part because businesses with 10 or fewer employees are not required to keep OSHA injury and illness records, Dr. Levin says.
The U.S. Centers for Disease Control and Prevention (CDC) seemed to confirm that underreporting with a study – coauthored by Dr. Patel at DSHS – showing far more cases of silicosis in the engineered countertop industry than previously believed. It showed that four states – Texas, California, Colorado, and Washington – independently confirmed 18 cases of silicosis, including two deaths, among workers in the industry between May 2018 and April 2019. Previously, only one instance of silicosis in the industry – a 2014 case from Texas – had ever been reported (tma.tips/SilicosisStudy).
“There is a sense that there is a broader problem existing out there that has not been adequately assessed because of a lack of reporting,” Dr. Levin said.
A 2008 study by the U.S. House of Representatives found that “work-related injuries and illnesses in the U.S. are chronically and even grossly underreported. As much as 69% of injuries and illnesses may never” be reported. Despite some changes made since, a 2018 report by the U.S. Department of Labor’s inspector general found OSHA data on workplace injuries and illnesses are still deficient and so are its assurances that employers have dealt with hazards.
Employees often are reluctant to self-report workplace injuries and illnesses, Dr. Levin says. Also, immigrants in some jobs are afraid of losing work or feel they have few options for making complaints.
“There are a lot of vulnerable populations that experience this kind of exposure that don’t surface through a reporting mechanism. Pesticide [poisoning among agricultural workers] is a good example,” he said. “These important issues of work-related exposures causing injury and illness may never see the light of day in the absence of reliable reporting.”
Job No. 1: Patient histories
Given this, physicians’ role in identifying potentially dangerous working conditions becomes more important than ever, Dr. Levin says. There often are few other ways to assess the severity of workplace injury and illness risk without considering occupational causes or reporting.
“We report infectious diseases [in part] to contain an epidemic,” he said. “For occupational exposure, one reason we report is to identify where there are sources of exposure and how to intervene in future exposure.”
Physicians report infectious diseases to their local or county health authority, which reports the data to DSHS and on up to CDC. Workplace illness reporting works differently because physicians send their information directly to DSHS. (See “Reporting Workplace Illnesses in Texas,” below). For example, lead exposure reporting usually comes from laboratories that do blood tests on patients, Dr. Patel says. But silicosis, asbestosis, and pesticide poisoning generally are reported by physicians.
With the growth of electronic health records and the growing awareness of the impact of occupation and ZIP code as social determinants of health, including this information in medical records can help with forming a diagnosis, reporting, surveillance, and research, Dr. Ball says.
Physicians should tell patients to describe their work history in their initial paperwork or try to go over that history in an early exam, Dr. Ball says. Physicians also should get background on the patient’s geographical history – where they’ve lived and for how long.
And physicians also should keep in mind the wide range of occupational illnesses and injuries patients can contract, Dr. Patel says.
“It’s not just these four reportable conditions,” she said. “Whenever physicians are consulting with their patients, work is an important part of an adult life. So getting more information about their exposures, whether it’s pesticide or silica or asbestos or even some ergonomic issue, it’s definitely important to capture that to provide a more holistic approach to patient care.”
With that background, physicians have a greater index of suspicion about other factors to investigate, such as workplace or environmental conditions, says Dr. Ball. Yet, establishing causation or even a strong association can be difficult because illnesses can have many causes. Factors such as smoking or chronic allergies may complicate a diagnosis, for instance.
Workplace illnesses tend to come with added layers of hassle for patients as well. Those illnesses often are not covered by typical health insurance plans, Dr. Ball says. And for worker’s compensation insurance, cases of silicosis and asbestosis in Texas have to be certified by a radiologist who is a “B reader” – someone certified by the National Institute for Occupational Safety and Health to diagnose workplace illnesses. Currently, there are only 10 such B readers in Texas and 175 in the U.S., according to the CDC.
With more detailed information, physicians can better help patients who come in with workplace illnesses like silicosis and pesticide poisoning – and provide more accurate data on those diseases, Dr. Ball says.
Tex Med. 2020;116(1):38-40
January 2020 Texas Medicine Contents
Texas Medicine Main Page