Emergency physicians spend nearly as much time documenting care as delivering it – but Stephen Stewart, MD, is using artificial intelligence (AI) to shift the balance back toward saving lives.
Documentation requirements often pull clinicians away from patients and extend work long after a shift ends. Emergency department physicians spend a median of 6.82 minutes per encounter on electronic health record (EHR) documentation, according to a 2024 study in JAMA Network.
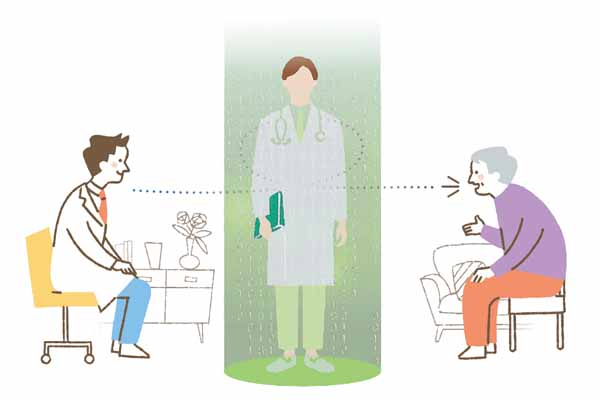
Dr. Stewart says AI documentation tools reduce that burden for him by creating a first draft of what happens in exam rooms, without requiring dictation or keyboard input. Dr. Stewart, who splits his time between a level one trauma center in Lubbock and a critical access hospital in Pagosa Springs, Colo., uses a HIPAA-compliant AI tool to record and document patient visits.
During patient encounters, with their consent to use the AI tool, he places his phone nearby, where the AI record conversations, transcribe them in real time, and automatically generate clinical notes within the EHR – allowing him to “focus entirely on the patient in front of him.”
After he explains his use of the technology, Dr. Stewart says his patients are mostly in favor of him using AI during their visits – even those who aren’t entirely in favor of the technology in other situations.
“I’ve had a few patients ask about it, and one recently said she really didn’t like AI,” he said. “I made it clear the AI is just summarizing our conversation and not making any medical decisions. She didn’t object to me using it.”
The system uses what is called natural language processing – a branch of AI that works to understand, interpret, and generate human language – to identify medically relevant details, such as symptoms and treatment recommendations, and organizes them into a document physicians like Dr. Stewart can then review and approve. That way, Dr. Stewart can provide patient care with a more hands-on approach – or, in this case, a “hands-free” approach, he said.
The AI tool has proved especially useful during fast-paced emergency visits, he says. For example, Dr. Stewart has relied on his AI documentation tool when treating a patient with lacerations requiring immediate attention. The AI captured his discussion with the patient while he was busy suturing and then turned that conversation into a clear procedure note.
“By the end of the visit, the AI had already captured my treatment plan and after-care instructions,” he said. “It’s just me and two nurses out at the hospital in Colorado. If I was having to do the charts manually, there’d be a lot more patients waiting for care. And secondly, I’d be staying a lot later after my shift to get my documentation done.”
Dr. Stewart discloses his use of AI to patients before every appointment to aid in complying with Texas law, which requires certain disclosures when AI is used for diagnostic purposes, including recommendations on a diagnosis or course of treatment, as well as when a patient “interacts” with an AI tool. After reading a Texas Medicine Today article detailing disclosure requirements, he began sharing a disclosure in his patients’ portals.
Dr. Stewart also uses ChatGPT to write discharge instructions for patients. However, he never puts patients’ protected health information into ChatGPT, as the platform is not HIPAA compliant.
To do this, he replaces all patient identifiers – including name, date of birth, and address – with general placeholders. This prompt could read, for example, as something as general as “middle-aged male presenting with high blood pressure.”
ChatGPT then generates a discharge summary that includes potential lifestyle modifications and follow-up care. Although Dr. Stewart admits he had to heavily edit AI’s work in the first few months of utilization, he’s now finding that the AI is “getting better and better,” especially as physicians train the technology.
However, Dr. Stewart said physicians still need to treat the technology as a “drafting tool, rather than a reference.”
“The key is to treat AI as an assistant,” he said. “But there are a lot of things that just aren't focused on emergency medicine, so we have to figure out how we can use tools made for others in ways that still work for us.”
For more information, the Texas Medical Association offers its members free resources within its artificial and augmented intelligence resource hub, including an AI vendor evaluation tool and information on the technology.
Alisa Pierce
Reporter, Division of Communications and Marketing
(512) 370-1469