
After 45 years in rural independent practice, Haskell family physician C. Wayne Cadenhead, MD, closed his office doors for the final time in late December 2023.
The last straw: successive Medicare physician pay cuts that had cratered the practice’s financial viability and made it near impossible to recruit staff at competitive wages.
“I’ve had enough,” he told Texas Medicine in his practice’s final days.
Dr. Cadenhead’s practice used to have four physicians as well as the capacity to perform surgeries and obstetric services. But it dwindled in recent decades, alongside Medicare physician payments.
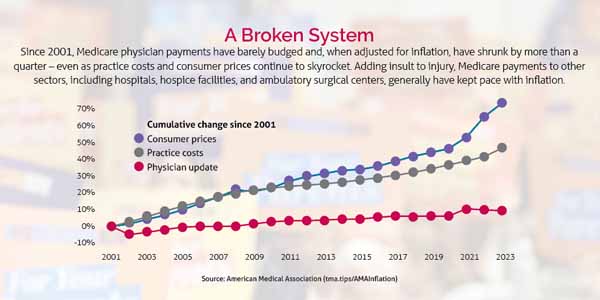
Between 2001 and 2023, such payments decreased by 26% when adjusted for inflation, according to the American Medical Association. (See “A Broken System,” page 21.) Over the same period, the consumer price index for physicians’ services in U.S. cities increased 65%.
Initially, Dr. Cadenhead supplemented anemic Medicare payments by working overnight shifts at the local emergency department. But at age 74, he had to cut back.
Without the additional revenue stream, the practice’s financial challenges – including keeping up with medical liability insurance and staffing – worsened.
“We [were] loosely surviving on my retirement funds and what private pay we [got],” he said.
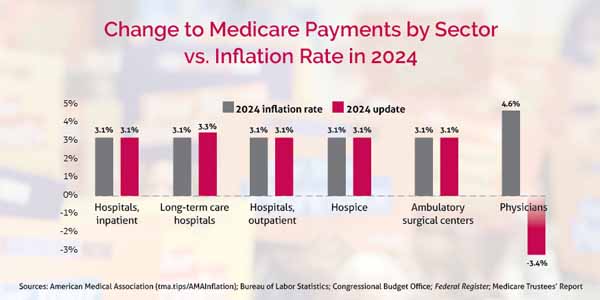
Dr. Cadenhead had hoped to remain open through July 2025, when he will turn 75 – the same age his physician father was when he closed his own private practice in Haskell. But the prospect of another Medicare physician pay cut – this time a nearly 3.4% reduction that took effect on Jan. 1, 2024 – made the decision for him and his patients, whose remaining care options are the county hospital or a handful of family physicians practicing in a 30-mile radius.
The cut stems from the 2024 Medicare physician fee schedule, which, like its predecessors, further erodes physician payment. Unlike in previous years, however, and despite a groundswell of physician advocacy, Congress failed to stop it or to heed medicine’s request for comprehensive reform when lawmakers passed a stopgap spending bill on Jan. 18. The measure fended off a federal government shutdown until early March but set off a cascade of Medicare-related consequences.
As this article went to press, a federal budget bill was in the works, and medicine has not let up the pressure on Congress to act on the Medicare cuts.
Even if not closing or retiring early, many physicians will be forced to reduce available health care services, cut practice hours, or even forgo treating Medicare patients altogether, as the Texas Medical Association, AMA, and others in organized medicine repeatedly warned during a months-long advocacy campaign.
“The inability of Congress to meaningfully address flawed Medicare physician payment policies, combined with rising costs, critically threatens our Medicare patients’ access to health care,” TMA President Rick Snyder, MD, said in a Jan. 19 statement. “What’s worse is how short-sighted Congress’ inaction is: These poor Medicare payment policies ultimately will cost America more because they are forcing doctors out of the system, thereby leaving patients no other option than to seek care in more expensive places.”
Speaking to a standing-room-only crowd at TMA's Leadership Summit in late January, AMA President-Elect Bruce Scott, MD, lamented the indefensible cuts amid rising inflation and called for a “total revamp” of the Medicare payment system.
“It’s time to fix Medicare [payment] now,” Dr. Scott said. “If we don’t, it’s ultimately the patients who will suffer.”
Medicine continues to shore up support for short- and long-term solutions, which, if passed, will be too late for physicians like Dr. Cadenhead and their patients. But these solutions could spare other practices from the same fate and preserve vulnerable patients’ ability to find care. At the very least, the fee schedule enacts other changes, some of them positive.
Most notably, the Centers for Medicare & Medicaid Services (CMS) heeded TMA’s pleas to mitigate changes to the Merit-Based Incentive Payment System (MIPS), whose potential penalties only exacerbate physicians’ payment woes. (See “Medicine’s MIPS Win,” page 24.) As a result, the MIPS threshold to avoid a penalty will remain unchanged in the 2024 performance year, providing much-needed stability to participants.
Other positive changes championed by TMA affect telemedicine – such as maintaining payment, supervision, and site flexibilities – and coding, including the addition of a new add-on “G-code” for complex visits.
MIPS Program Stabilized in Medicare Fee Schedule
Telemedicine Flexibilities Preserved in Medicare Fee Schedule
Coding Changes in Fee Schedule Promote More Accurate Payment for Complex Visits
The high cost of low payments
The 2024 fee schedule lowers the conversion factor that determines physician payments by nearly 3.4% compared with the 2023 formula, continuing a long-standing trend that “harm[s] practices trying to stay viable and care for the most vulnerable patients – older adults and people with disabilities,” Dr. Snyder wrote in September 2023 in one of a series of letters in which TMA, AMA, and dozens of physician organizations pleaded with Congress to intervene.
Congress often passes stopgap legislation in late December or early January to mitigate the fee schedule cut. But this annual rigmarole only adds to the strain on physician practices, says Gary Sheppard, MD, an internist in Houston and chair of TMA’s Council on Socioeconomics.
“From a business standpoint, you take the worst-case scenario” – that Congress doesn’t act and the cut remains wholly in place – “and you ... plan with that.”
For some physicians, planning for the worst-case scenario means no longer accepting new Medicare patients, leaving private practice for employment, moving away from a rural area, or shutting down their practice. For patients, it means fewer care options.
“These are the hard decisions that have to be made,” Dr. Sheppard said.
In its vociferous efforts to get Congress’ attention, TMA heard from dozens of Texas physicians in such dire straits.
“All the doctors I have referred patients to are leaving or gone,” lamented Denton obstetrician-gynecologist Laura Finger, MD.
“If this additional [Medicare] payment cut goes through, in the midst of inflation and COVID causing rising costs for staff salaries and benefits, I would have no choice but to stop caring for these patients,” a worried Dallas-Ft. Worth physician told TMA in December.
“I’m terrified for what this will mean for my elderly patients and their access to care,” another doctor, from Central Texas, shared.
TMA President-Elect Ray Callas, MD, an anesthesiologist in Beaumont, worries that further reductions to Medicare physician payments jeopardize the entire program at a moment when demand for its services is growing. By 2030, the entire baby boomer generation – those born between 1946 and 1964 – will be eligible for Medicare, according to the U.S. Census Bureau.
One practice TMA heard from calculated in late 2023 that, if the January 2024 cut were enacted, “our [Medicare payment] rate will be lower than what we received in 2012.”
A Dallas physician calculated even worse: “My Medicare [payment], factoring for inflation, is less than half of what it was in 1998.”
Dr. Callas lays out a domino effect: Medicare physician pay cuts lead to physician practice closures. Physician practice closures mean Medicare patients lose access to health care. Loss of access to health care means Medicare patients grow sicker. Sicker patients seek out care in emergency departments. And emergency department use drives up health care spending.
“We know the Medicare system is a failing system, and it’s not sustainable,” he said.
In recent years, TMA’s advocacy strategy has grown to encompass comprehensive reform of the Medicare physician payment system as well as efforts to avert individual cuts. The association continues to urge immediate congressional action on federal legislation that would reverse the 2024 fee schedule cut and prevent others like it in the future.
“TMA will not let up in its efforts to protect Texas patients and physicians from these ongoing, harmful cuts,” Dr. Snyder said in the Jan. 19 statement. “Congress must act now to resolve this decades-old problem.”
For now, TMA remains focused on two bills.
In the short term, the Preserving Seniors’ Access to Physicians Act of 2023 (House Resolution 6683) by U.S. Rep. Gregory Murphy, MD (R-N.C.), would eliminate the nearly 3.4% cut that took effect earlier this year. The bipartisan bill is co-sponsored by U.S. Reps. Michael Burgess, MD (R-Texas); Larry Bucshon, MD (R-Ind.); Danny Davis (D-Ill.); Jimmy Panetta (D-Calif.); and Brad Wenstrup (R-Ohio).
In pursuit of a long-term fix, TMA also continues to champion the bipartisan Strengthening Medicare for Patients and Providers Act (House Resolution 2474) by U.S. Rep. Raul Ruiz, MD (D-Calif.), which would provide annual inflation updates to the Medicare physician fee schedule in line with the Medicare Economic Index, a measure of practice cost inflation, among other reforms. The bill has been a topic of discussion at several recent congressional hearings in both chambers.
“These bills show members of Congress have the desire to fix this problem and have multiple solutions at their disposal,” Dr. Snyder said. “We just need Congress to act for the sake of our vulnerable patients.”
Dr. Callas stresses the importance of this two-pronged approach, which could break the cycle of regular Medicare physician pay cuts. This cycle stems from federal budget-neutrality provisions that mandate any physician pay increase or decrease be offsetting.
When Congress intervenes, the fee schedule cut often is reduced but not eliminated, he adds. For small and solo practices, and especially those in underserved areas, such cuts can imperil their already razor-thin operating margins.
“Every time we ask for a Band-Aid, we still get a scratch,” he said.
To secure legislative relief, Dr. Callas says medicine relies on sustained physician advocacy. He encourages his peers to reach out to their representatives at the local, county, state, and federal levels to educate them about what’s at stake.
“We’ve got to be boisterous,” he said.
Dr. Callas also urges physicians to speak with their Medicare patients, who might help amplify their message to Congress.
“Physicians touch one thing that’s important to legislators,” he said. “Physicians touch patients, and patients are voters.”
Dr. Sheppard agrees, saying that the 2024 Medicare physician fee schedule and the process that produces it imperil physician practice viability and patient access to care.
“We don’t want patients to suffer,” he said. “If we don’t stop the changes and the cuts and everything else, you [lawmakers] are going to find your constituents don’t have anyone to see.”