
Sidney Ontai, MD, was into telemedicine before telemedicine was cool.
In 1995, while still in academic medicine, he got a grant from the National Library of Medicine to help set up telemedicine on Catalina Island, off California. That familiarized him with both the technology and the complicated billing procedures.
“So when I got out of academia and hung out a shingle in 1999, I knew I could do this,” said Dr. Ontai, a former chair of the Texas Medical Association’s Committee on Health Information Technology (HIT). “It was just kind of a hobby almost.”
Dr. Ontai set up his private practice in the panhandle town of Plainview, about midway between Amarillo and Lubbock, and added a telemedicine clinic about 60 miles away in a tiny town that the U.S. Department of Health and Human Services designated as a health professional shortage area. Dr. Ontai’s “hobby” telemedicine clinic put him squarely on the cutting edge of medicine.
“When I first set this [clinic] up in Turkey, Texas, in 2001, that little clinic was responsible for 20 percent of Medicare’s telemedicine visits – because nobody else was doing it,” he said with a laugh.
Fast forward 18 years, and telemedicine has changed quite a bit. For starters, the technology is better, says Dr. Ontai, who now practices in Victoria, near the Gulf Coast. Instead of needing bulky, expensive cameras and screens, just about anyone with a computer and a HIPAA-compliant teleconferencing app can get started.
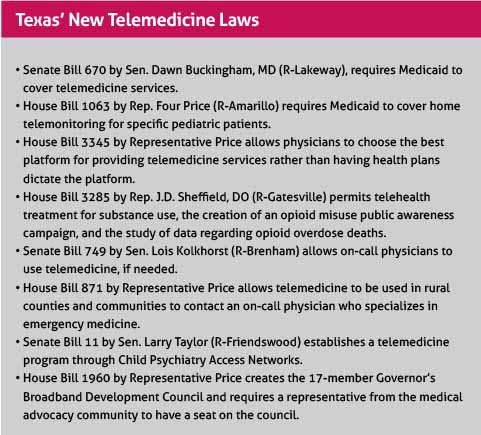
The billing is still overly complicated, however. Payers have always been inconsistent about what they pay for telemedicine, but that is getting better, thanks in part to new state laws backed by TMA, like one that requires Medicaid to cover services provided via telemedicine. (See “Texas’ New Telemedicine Laws,” page 28.)
Telemedicine overcomes many obstacles to health care – mostly by bringing the expertise centered in big, regional medical centers to small towns like Turkey (population 389). In 2018, 34 Texas counties out of 254 had no primary care physicians, and 110 had five or fewer, according to the Texas Department of State Health Services.
“We’re using telemedicine more because it’s just such a rational solution to distance and problems with [health] care,” says Billy Philips, PhD, who oversees the extensive telemedicine program the Texas Tech University Health Sciences Center (TTUHSC) runs in Lubbock.
Telemedicine reaches other hard-to-reach populations as well, including prisoners, victims of natural disasters, and elderly shut-ins. It’s also growing because of the convenience it provides patients, especially for routine visits. About 70% of patients are interested in receiving a range of health services virtually, but only 20% have experienced virtual health care, according to a 2017 report by Accenture, a professional services company.
“Over the next six years, virtual visits will overtake in-person visits [nationally], and the average doctor is completely unprepared for this reality,” said Clint Phillips, CEO of the telemedicine provider Medici, referring to a 2017 article by researchers from the University of Rochester Medical Center (tma.tips/Telemed
Future).
But a growing number of physicians are embracing telemedicine.
Because most physicians still have no first-hand experience with it, they have many questions about how it will help them and their patients. The answers can vary from specialty to specialty, but however it’s employed, telemedicine definitely helps any medical practice extend its reach, says John Griswold, MD, a Lubbock burn specialist who helped pioneer telemedicine in Texas.
“Once you do it, you realize it’s a very comfortable way to do health care,” he said.
Step 1: Assessing needs
Telemedicine takes on several forms. Sometimes it involves simply collecting or transmitting medical information, like radiology or diagnostic records. Also, many physicians can now consult on a patient’s case remotely with more experienced physicians. (See “ECHO-ing Across Texas,” February 2019 Texas Medicine, pages 44-46, www.texmed.org/ECHO.)
New technology allows physicians to monitor patients with chronic conditions like diabetes or asthma remotely, allowing faster response times in emergencies. More typically though, telemedicine involves real-time doctor-patient visits that are conducted with the help of cameras and viewing screens.
Some medical specialties use telemedicine more than others. An American Medical Association study published in December 2018 reported that 39.5% of radiologists use telemedicine, more than any other specialty. They were followed by 27.8% of psychiatrists and 24.1% of cardiologists. In Texas, the majority of telemedicine and telehealth services are used to treat patients with behavioral health conditions, according to the Texas Health and Human Services Commission (HHSC).
Physicians contemplating telemedicine need to first assess how it is going to help their patients, says Dr. Griswold, director of the Timothy J. Harnar Burn Center in Lubbock, a Level 1 trauma center. In the late 1990s, Dr. Griswold needed to find a better way to do follow-up visits for burn surgery patients. Many had already traveled hundreds of miles to Lubbock for their surgery, and making a return trip for follow-ups was too difficult.
Dr. Griswold set up a telemedicine clinic in El Paso through TTUHSC. Patients in far west Texas could go there to be examined remotely and avoid the long trip to Lubbock. Because examining burned skin is mostly visual, the clinic was a perfect solution, and it quickly led to faster recovery times and fewer hospital readmissions.
“Probably the biggest thing we noticed is the improvements in the patients’ recovery,” Dr. Griswold said.
Step 2: Payment
Once physicians figure out how telemedicine can help patients, they must wrestle with the issue of payment. Since the late 1990s, the Texas Legislature has passed more than a dozen laws that have gradually removed barriers to telemedicine and made it more profitable for physicians. In 2017, for instance, a TMA-backed bill removed the requirement for having an in-person meeting to establish a physician-patient relationship. Instead, it mandates that physicians meet the same standard of care as that required for an in-person visit.
That and other reforms led to a 30% jump in the number of Texas patients using telemedicine and a 32% increase in the number of health care professionals using it between 2016 and 2017, HHSC reported. New laws passed with TMA’s support in the 2019 legislative session will make telemedicine even more attractive to physicians and patients, Dr. Philips at TTUHSC says.
Yet payment still can be confusing, says Ogechika Alozie, MD, an El Paso infectious disease specialist who is vice chair of TMA’s Committee on HIT. Most forms of insurance do not pay physicians as much for a telemedicine visit as an in-person visit.
“It’s just not clear what you’re going to get from what you bill,” he said.
Given this lack of transparency, collecting payment directly from the patient at the time of the service remains the easiest way to pay for visits via telemedicine, says Dr. Alozie, who also sits on TMA’s newly formed Telemedicine Task Force. Most physicians charge between $20 and $150 for a virtual visit, depending on their specialty and the complexity of the case, according to telemedicine company Medici.
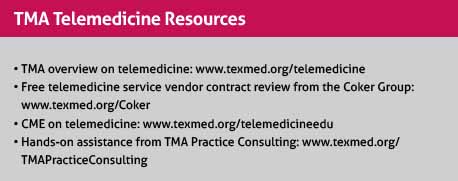
TMA provides resources that can help physicians navigate these and other difficult aspects of telemedicine. (See “TMA Telemedicine Resources,” page 29.) Also, TTUHSC’s TexLa Telehealth Resource Center is a federally funded program that provides technical assistance, including education on payment matters (www.texlatrc.org).
Step 3: Finding a steady platform
Next, physicians should look at how to make telemedicine work technically: finding the right equipment and the right telemedicine provider. Both are specific to the individual physician’s needs. Some gadgets and telemedicine providers are better for video conferencing while others are better for messaging or physician-to-physician consultation.
Choosing the correct platform became much easier thanks to the 2019 passage of TMA-supported House Bill 3345 by Rep. Four Price (R-Amarillo), which allows physicians – not the health plans – to choose the best platform for them.
“We’re really excited about that, because it allows the [physicians] to say, ‘This is what I want to put my patients on,’” Dr. Alozie said.
But all telemedicine platforms come with drawbacks, he says. For instance, some still do not directly integrate with electronic medical record (EMR) systems, meaning the physician has to transfer notes and other information manually to the EMR.
“I look forward to the day when these platforms and the EMR vendors work on … direct integration so that you can use whatever tool or vendor you want and it shows up on the screen and you can do the work on your EMR,” he said.
Physicians attempting to understand telemedicine should identify the amount of time they can devote to it, set aside blocks of time just for those patients, and start off small, Dr. Alozie recommends.
“Don’t try to bite everything off at once and switch 30 to 40 percent of your practice’s workflow into telemedicine upfront,” he said. “Make sure you’re not losing time and money just because of a desire to be technologically advanced.”
Telemedicine at its worst is when the “tele” part does not work, says Frances Ebo-Anagor, MD, a second-year resident working in a Texas A&M Health Science Center residency program overseen by Dr. Ontai. Dr. Ebo-Anagor helps with the clinic in Turkey and clinics in three other small towns scattered between Lubbock and Amarillo.
“When you’re trying to talk to the patient and the computer or system disconnects … that causes a real disruption in the flow of care,” she said.
Nevertheless, she’s glad she’s getting trained on telemedicine and plans to use it when she sets up her own practice.
“It’s going to grow … and it provides better quality care” for hard-to-reach patients, she said. “But we have to make it more accessible and more affordable so individual physicians can incorporate that into their practice.”
Tex Med. 2019;115(8):26-29
August 2019 Texas Medicine Contents
Texas Medicine Main Page