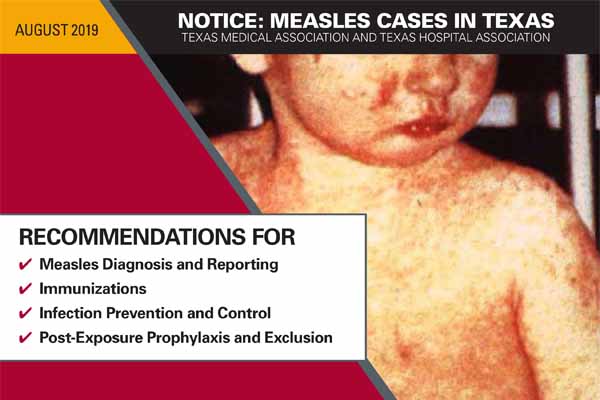
As measles cases continue to rise in Texas and across the U.S., the Texas Medical Association and Texas Hospital Association have created a document to help physicians and other health care professionals combat the highly contagious respiratory illness.
The document provides the latest recommendations for diagnosing and reporting measles, immunizations, infection prevention and control, and post-exposure prophylaxis and exclusion.
The information is adapted from the California Department of Public Health’s All Facilities Letter (AFL) Summary published in April.
As of late July, officials have confirmed 21 measles cases this year, including six in El Paso County, six in the Dallas-Fort Worth area, and four in Harris County. Nationwide, more than, 1,164 measles cases have been reported, the greatest number of cases in the past 25 years.
“Measles is highly communicable and is spread by airborne and contact methods. Hence, promptly identifying measles cases and implementing control measures immediately can reduce the risk of measles transmission and avoid the need for epidemiological investigations of potential health care contacts,” the joint TMA/THA document says. “Consider measles in patients of any age who have a fever and a rash, regardless of their immunization history.”
Physicians, health care providers, hospitals, and other health care facilities must report all confirmed and suspected cases immediately to (800) 705-8868, or to their local or regional health department.
Physicians should encourage their patients to immunize themselves and their children against the disease. The vaccine is called the “MMR” vaccine because it also protects against mumps and rubella.
The Centers for Disease Control and Prevention (CDC) recommends:
- Children should receive two doses of MMR vaccine – at age 12 through 15 months, and at age 4 through 6 years, or at least 28 days after the first dose.
- Students at post-high school educational institutions who do not have evidence of immunity need two doses of MMR vaccine, separated by at least 28 days.
- Adults born in 1957 or later who do not have evidence of immunity should get at least one dose of MMR vaccine.
- Health care personnel who do not have presumptive evidence of immunity should get two doses of MMR vaccine, separated by at least 28 days.
The TMA/THA resource also provides best practices to prevent and control the spread of the disease when caring for suspected patients.
Ideally, suspected patients should be placed in an airborne isolation room, if possible. If an airborne isolation room is not available, patients should be masked immediately and should not be allowed in waiting rooms or other common areas.
In addition, only health care personnel with documentation of two doses of live measles vaccine or laboratory evidence of immunity should be allowed to enter the patient’s room.
“If the patient was not immediately placed in an airborne isolation room, make note of the staff and other patients who were in the area during the time the suspected measles patient was in the facility and for at least two hours after the suspected measles patient left,” the notice says. “If measles is confirmed in the suspected measles patient, potentially exposed people will need to be assessed for measles immunity.”
More information can be found in the CDC’s Guideline for Isolation Precautions.
TMA’s Be Wise – ImmunizeSM webpage also provides plenty of resources to help prevent measles and other infectious disease outbreaks, and educate patients on immunizations.
Additionally, TMA’s website contains useful information to help you talk to your patients about the measles vaccine, including a video and informational poster you can print out and hang in exam rooms.