Odessa allergist and immunologist Vivek Rao, MD, is something of an outlier.
Well below retirement age at 49, he is younger than the average age of physicians in his specialty and in his region. Although Odessa is a metro area, it is surrounded by rural counties, and he regularly sees patients who drive hours to see him for lack of specialty care options closer to home.
Dr. Rao worries about these patients, who relay to him their concerns, including a dearth of primary care and specialty physicians and rising health care costs that cause them to delay care until it’s urgent or emergent. He also frets about the enduring challenges of recruiting physicians to Odessa and more rural places, which lack the amenities, population density, and higher share of privately insured patients of major cities.
“The main reason I’m practicing in Odessa today is the fact that I grew up here,” he told Texas Medicine. “What made me want to return to Odessa to practice medicine was the need here for physicians.”
This need is evident, according to the Texas Medical Association’s Committee on Physician Distribution and Health Care Access, which just submitted its annual workforce update to the association’s House of Delegates, set to meet in May.
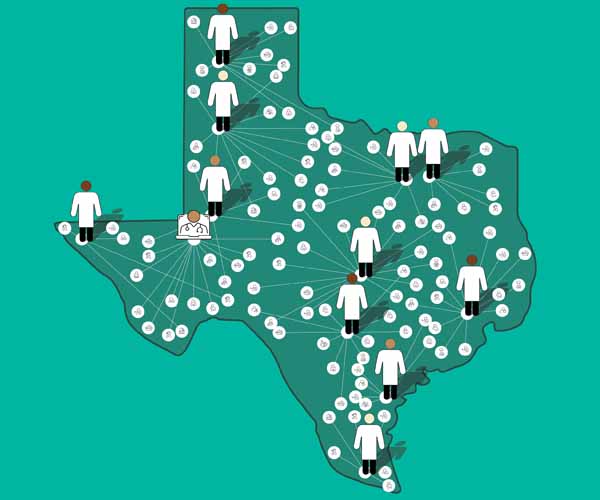
Texas’ physician supply continues to outpace the state’s rapid population growth. But the state lags in its ratio of patient care physicians, at an average of 198 per 100,000 people versus the U.S. average of 252.
Meanwhile, an increasing average physician age foreshadows a deepening workforce crisis. Texas’ shortages range across specialties, and, for 23 of those specialties, at least one-third of their Texas workforce is over age 55, indicating “the greatest need for recruitment in the next five to 10 years” as these physicians approach retirement, TMA’s report said.
While the study highlights positive growth facilitated by TMA’s ongoing advocacy, it shows shortages that mirror those across the health care professional workforce and that are particularly entrenched in rural areas. (See “Texas’ Physician Workforce,” page 18.) It also reveals challenges brought on by the COVID-19 pandemic and by other factors, economic or otherwise, that have complicated Texas’ practice environment and impacted recruitment.
Fortunately, TMA has a long track record of success advocating for legislative solutions to the state’s physician workforce challenges. The 2003 medical liability reforms TMA championed continue to attract physicians to Texas. Since then, the association has secured increased funding for medical schools with a focus on rural and underserved areas and for residency training programs in select specialties, seeding the wins detailed in its latest report.
“I am encouraged for the first time in quite a while that the recent legislature may have a positive impact on the rural workforce,” said Stephen Whitney, MD, a pediatrician in Missouri City who chairs TMA’s Committee on Physician Distribution and Health Care Access.
TMA built on this progress last year, when lawmakers continued their investment in sustainable workforce solutions that maintain Texans’ access to high-quality, physician-led care through increased funding for graduate medical education (GME) and loan repayment programs, broadband expansion, and the Texas Medical Board. TMA also worked last session and continues to work to mitigate the maze of Texas’ complex vaccine and abortion laws, which physicians say have challenged recruitment in related specialties, and to stamp out scope-of-practice creep.
In tandem with preventing such scope creep, TMA’s top priority during the 2023 regular state legislative session was to address physician workforce shortages in a way that ensures patients have access to the same high standard of care, regardless of their location. Thanks to a multipronged advocacy strategy, TMA was successful, stymying more than 130 scope-related bills and securing significant budget gains that will expand access in the short term while shoring up the physician workforce in the long term.
“A lack of physicians is not going to be made up by supplying more nonphysicians to take our place because the gap in education and experience is too much,” said TMA’s 2022-23 President Gary Floyd, MD, a pediatrician in Corpus Christi. “To gain more physicians, one of our best strategies is to make our own.”
TMA’s report is the first issued since the wind-down of the COVID-19 pandemic, which has factored into Texas’ workforce in both positive and negative ways.
On the one hand, the pandemic ushered in the widespread adoption of telemedicine as well as the necessary regulatory flexibilities to facilitate that shift, which has helped improve access to care. (See “Valuable Screentime,” page 20.)
On the other hand, the major public health emergency had a deleterious, knock-down effect on Texas’ overall health care professional workforce and drove pent-up demand for health care services, says Nancy Dickey, MD, a family physician in College Station and president emeritus of the Texas A&M Health Science Center.
“The pandemic certainly seemed to be accompanied by a complimentary epidemic of burnout of health care workers,” the past president of the American Medical Association told Texas Medicine. “In [areas] with a perpetual shortage, that obviously made it worse.”
Burnout is one reason Texas’ infectious diseases specialty workforce – already disproportionately small compared with the state population and concentrated in metro areas – is reeling at this stage of the pandemic, says Susan McLellan, MD. The infectious disease specialist in Galveston, who serves on TMA’s Committee on Infectious Diseases, also cites low pay and other pressures, like vaccine hesitancy.
In response, TMA’s House of Delegates approved a resolution during TexMed 2023 directing the association to, among other things:
- Strengthen the infectious diseases specialty workforce, such as by encouraging the development of peer-to-peer consultation models; and
- Advocate for infectious diseases specialty care payment reform.
TMA also is tracking a historic dip in interest in emergency medicine among medical students in 2023 following the pandemic, as well as reports of the loss of obstetrician-gynecologists from the state and declining interest among medical students to train in this specialty, the report states.
The pandemic also seriously challenged practice viability. Meanwhile, a confluence of other economic factors like decreasing pay, especially in primary care, continues to take a toll on Texas’ physician workforce, Dr. Whitney says.
For one, industry consolidation has driven many physicians toward employment and away from independent practice, where just 34% of Texas physicians remain, according to the Physicians Advocacy Institute. Independent practices in rural areas face the same economic headwinds as their urban counterparts, plus the added challenges of an older, poorer patient population and more acute staffing shortages across the health care team.
Dr. Whitney also cites increasing pressure from Medicare. Between 2001 and 2023, Medicare physician pay decreased by 30% when adjusted for inflation, even as Medicare payments to other sectors generally kept pace, according to AMA. Over the same period, the consumer price index for physicians’ services in U.S. cities increased 65%.
As TMA and its allies have repeatedly warned lawmakers, any cut risks practice closure, early retirement, and reductions in health care services or office hours.
Such factors continue to threaten practice viability and patient access to care – 23 rural Texas counties had zero primary care physicians in 2022 and in 2017, according to TMA’s report. On top of that, inadequate payment incentivizes medical students – 67% of whom graduate with debt, according to the Association of American Medical Colleges – to choose higher-paying specialties, which tend to be concentrated in metro areas.
For these reasons, Robert Emmick, MD, an emergency physician in Austin and past chair of TMA’s Committee on Physician Distribution and Health Care Access, lauds TMA for championing new medical schools and residency slots in rural and underserved areas as well as increased funding for medical school loan repayment programs that incentivize residents to train in the same areas.
While such interventions take time to produce results, 80% of Texas medical school graduates who complete their residency in state remain here to practice, Dr. Floyd says.
“To do that, we need increased medical schools, which we’ve done ... and to make sure we have adequate training and residency programs.”
Dr. Whitney added: “If you can get somebody to spend a few years in a community, they form significant ties,” which may be enough to get them to stay.
TMA has long advocated for diverse investments in Texas’ rural physician workforce pipeline, which have paid off with the recent openings of two new medical schools – Sam Houston State University College of Osteopathic Medicine in Conroe in 2019 and UT Tyler School of Medicine in 2023 – dedicated to addressing the shortage in East Texas.
In addition, the Texas Legislature budgeted $233 million for the 2024-25 biennium – up 17% compared with the 2022-23 biennium – for the GME Expansion Grant Program. The program supports the creation of new residency slots necessary to maintain the target 1.1-to-1 ratio of slots to medical school graduates. Lawmakers also allocated $116 million – up 12% – to residency training programs sponsored by medical schools; this funding helps offset the cost of teaching residents.
- The Family Practice Residency Program, which received $16.5 million in 2024-25, up from $9 million in 2022-23. Its grants go to the state’s nationally accredited family medicine residency programs to increase the number of physicians who choose that specialty.
- The Physician Education Loan Repayment Program, which received $35.5 million, up from $29.5 million. The program incentivizes primary care physicians and psychiatrists to practice in rural and underserved areas by paying off their student loans.
- The Joint Admission Medical Program (JAMP), which received $11.7 million, up from $9.7 million. JAMP encourages economically disadvantaged students to pursue careers in medicine by offering scholarships, paid internships, mentorships, and other support.
- The Rural Residency Training Program, which received an inaugural allotment of $3 million. TMA initiated the 2019 creation of this program, which will issue grants to fund new residency positions in nonmetropolitan areas.
TMA also championed legislation that funded 30 new full-time positions at the Texas Medical Board, which maintains oversight of physicians and accommodates the influx of medical license applicants from other states, drawn in part by the TMA-backed medical liability reforms enacted in 2003.
Texas’ growing child and adolescent psychiatry workforce is another critical win given the “national state of emergency” in youth mental health, as declared in October 2021 by the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association.
David Lakey, MD, vice chancellor for health affairs and chief medical officer at The University of Texas System, says TMA and others in organized medicine have raised concerns about this specialty workforce shortage going back a decade.
Heeding this advocacy, the Texas Legislature in 2019 created the Texas Child Mental Health Care Consortium, which oversees the Child Psychiatry Access Network (CPAN) and the Texas Child Health Through Telemedicine program. The consortium also funds expansion of the psychiatric workforce, child and adolescent psychiatry fellowship programs, and improved mental health research. In 2021, the Texas Legislature expanded CPAN and created PeriPAN to address perinatal mental health and reduce maternal mortality and morbidity rates.
Dr. Lakey sees a direct connection between this funding and the growing specialty workforce, citing new fellowship programs at Texas Tech University Health Sciences Center Lubbock, the University of North Texas Health Science Center, and The University of Texas at Tyler as well as a new triple-board residency program at UT Southwestern Medical Center.
“We worked with the legislature for a while,” he said. “Mental health is one of the issues that affects everybody. Not only are their constituents impacted and challenged with getting mental health services, but frequently family members [also] are challenged with getting the services that they need.”
Looking ahead to 2025, TMA is focused on ensuring the Texas Legislature maintains such funding and finds new ways to grow and maximize the state’s physician workforce across the many specialties it needs.
Fortunately, Dr. Rao says the pandemic catalyzed not only telemedicine use but also tele-advocacy, making it easier for physicians like him – located far away from Austin – to support TMA and medicine-friendly policies. He encourages his fellow physicians to get involved in this effort if they haven’t already, given the high stakes for Texas’ physician workforce and the patients who rely on it for access to care.
“We need all physicians to be involved,” he said. “We need all hands on deck with this.”