
Texas Tech University Health Sciences Center (TTUHSC) School of Medicine student Asher George has known he’s wanted to pursue a career in medicine almost his entire life – but wasn’t always sure how to do so.
As a high school student, Mr. George participated in Stephen F. Austin State University’s Joint Admission Medical Program (JAMP) Camp, which allowed him to sit in on premedical classes, meet with medical professionals, and receive a firsthand look at what it’s like to work in hospitals, clinics, and other medical facilities.
JAMP Camp advisors then guided him in the right direction.
“I remember speaking to one of my fellow medical students from a small West Texas town and learned that her knowledge of how to get into medical school was through Google searches,” Mr. George said. “Especially how to take the MCAT [Medical College Admissions Test], what classes to take, what most medical schools look for in a prospective student. … For many students from rural areas this story seems to be very common, just because their resources are so limited.”
On the contrary, through JAMP, “I learned how to access resources to be an effective premed student,” he said. “That opportunity really helped me figure things out, especially as the first person in my family to go to medical school.”
Mr. George continued his medical education at Texas Tech through a summer rotation in Alpine, under the Texas Family Medicine Preceptorship Program. When starting his rotation, Mr. George was eager for opportunities to guide high school students, like the mentorship he experienced at JAMP Camp. So, he and his mentor, Adrian Billings, MD, director of the TTUHSC Permian Basin Alpine Rural Family Medicine Residency Track, created their own program, which has rapidly grown since.
“There’s definitely a gap between the urban physician population versus the rural population, and we’re not meeting that need,” said Dr. Billings, who also serves on the Alpine Independent School District Board of Trustees. “Many high schools in these rural school districts just don’t have the knowledge, funding, or the time to really focus on those kids who might be interested in medicine. If we’re going to improve the rural health care workforce, we have to target these rural kids, we have to enable them, and then we have to give them a chance.”
Texas is second in the nation for health professional shortage areas, says the U.S. Health Resources & Services Administration (HRSA), with rural populations suffering the most.
The Texas Department of State Health Services projects that within the next decade, Texas will lack over 10,000 full-time physicians.
To counteract these trends, rural physicians, medical schools, and medical students are partnering with their communities to create mentorship programs that reach local students early in their education and expose them to careers in medicine.
Mr. George believes that in addition to these programs, Texas should increase funding to create medical residency positions in rural areas.
“When you have a pipeline of students from a small hometown that are willing to go back to that area to practice, it really helps to provide a good look at what they can experience in the health care system as they progress through their educational career,” he said.
As residents often practice near where they train, per the Association of American Medical Colleges, and with many of Texas’ medical schools in big cities, many rural students become urban physicians. Out of the 16 medical schools in Texas, only a handful serve rural communities.
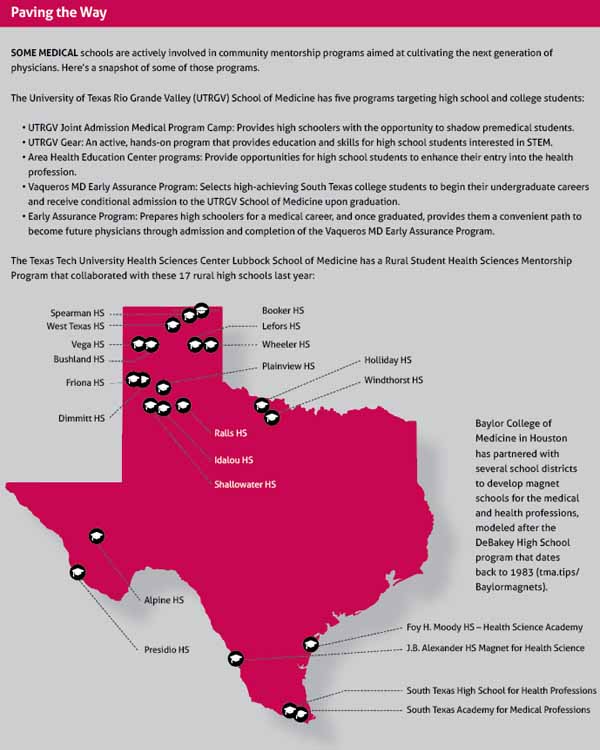
The University of Texas Rio Grande Valley (UTRGV) School of Medicine aims to change that.
As one of Texas’ newer medical schools, UTRGV was fortunate to start with the mission of “growing their own” and made community mentorship a part of that strategy from the beginning.
“The physician-to-patient ratio here is ridiculously low compared to the rest of Texas,” said Harlingen family physician and associate dean for diversity, inclusion, and health equity at UTRGV School of Medicine Adela Valdez, MD. She is also a member of TMA’s Council on Medical Education.
“Having UTRGV and its community programs here has made a huge difference in bringing care and education to this area. We know that physicians practice where they trained, and we want our students to not only become successful doctors but stay in this area and treat their community.”
TMA past President E. Linda Villarreal, MD, who practices in the Valley, believes that medical schools like UTRGV are some of the best facilitators of medical mentorship.
“With these programs, students have more exposure to the medical field that will enhance their desire to do what we do,” she said. “How can we help students? Well, if we can solicit volunteers from medical schools to become mentors, then young students won’t have to go to another geography to find resources.”
From student to mentor
The closest medical school to Alpine, Texas Tech Lubbock, however, is almost a five-hour drive away, a common reality rural students face when exploring interest in a medical career. It’s no wonder the internet is sometimes rural students’ only resource, Mr. George says.
“High school students in some of these small towns don’t have teachers, counselors, or mentors knowledgeable in the medical field to guide them into knowing how to approach undergraduate studies, and if they’re in college, what to do to become a doctor,” he said.
With only three primary care centers scattered across Alpine, and two in nearby Marfa, students in the area have few physicians to model their careers after and often are left to pave the way for the next decade of schooling themselves.
Moreover, Alpine and its surrounding areas fall within the Permian Basin, the second-largest shale gas-producing region in the U.S. Many students in the Permian Basin, Mr. George found, became uninterested in medicine following these challenges and often chose to pursue more visible careers within the industries around them.
“One of the biggest struggles in the Permian Basin is that there’s a lack of students attracted to the health care field,” he said. “Many of them will leave high school and enter the oil and gas industry, which creates a lack of health care professionals in the area. At the end of the day, these students don’t see enough men or women in white coats.”
Mr. George brought these concerns to Dr. Billings, his preceptor.
Dr. Billings wasn’t surprised by Mr. George’s concerns. As a rural-born resident turned physician, Dr. Billings is intimately familiar with the access-to-care struggles of nonurban patients and the desperate need to get more physicians to the area.
“There’s one family physician for 5,000 patients in the Big Bend area right now. That’s a delay of care,” Dr. Billings told the House Public Health Committee of the Texas Legislature in 2022. “That means sicker patients, that means more costly care. That means less productivity. That means more death.”
Together, Dr. Billings and Mr. George began working towards a solution to generate more interest among local youth in medicine: the Rural Student Health Sciences Mentorship Program, which connected medical students to rural high schoolers in need of medical mentorship.
“We needed a program to equip high school students with the knowledge of how to get into college, how to get into medical school, and what a day in the life of a medical student looks like,” Mr. George said. “Mentoring partnerships allow students to see what it’s like to go into health care. I started this program so that rural students could become future Texas doctors.”
Before the start of his second year of medical school, Mr. George took his plan to his medical school admissions department and the West Texas Area Health Education Center (AHEC), which coordinates pipeline activities to recruit and engage students to enter the health care workforce. West Texas AHEC provided the rural mentorship program with travel funding for mentors to meet with mentees at high schools across the region and partnered with rural schools to identify students interested in medicine.
Mr. George then began assembling fellow second-year medical students to oversee the needs of the mentor-mentee partnerships at their assigned rural high schools through monthly in-person or Zoom meetings. Mentor responsibilities included holding conversations with counselors and teachers on how to better prepare students for a career in medicine, supporting high school students by answering questions, providing information, and walking them step-by-step through the undergraduate and medical school process.
“This rural high school mentoring program was so needed because our rural students didn’t know of all the pathway and pipeline programs that are in existence,” Dr. Billings said. “And these students can really relate to a younger medical student that is much closer to college and taking the MCAT than to a senior physician far away from that process.”
The program officially began during the 2020-21 academic year with 30 second-year medical student mentors and 30 rural high school mentees. Now, it has grown to 40 medical students and 57 high schoolers across 17 rural high schools. (See “Paving the Way,” page 33.)
Zane Billings, Dr. Billings’ Alpine High School senior son, is one of those rural students who was given a chance.
“This has definitely opened my eyes and helped me to realize what’s in store going through the medical route,” Mr. Billings said.
Since his involvement, Mr. Billings has been accepted to the Texas Tech Honors College Undergraduate to Medical School Initiative of TTUHSC, which he plans to attend like his mentor, Mr. George.
“Asher, who was my mentor, guided me on the road to having a medical career. I didn’t even realize what I needed to do to have a competitive medical school application to ultimately get the residency and career I want until I was involved in this program,” Mr. Billings said. “I wish everyone had a mentorship program like ours.”
A Grande solution
Fortunately, Edinburg pediatrician Cristel Escalona, MD, was able to begin her medical mentorship much earlier – in fifth grade, in fact.
Dr. Escalona’s first mentor, her fifth-grade chemistry teacher, encouraged her not only to become a physician but also to stay and treat her community within the Rio Grande Valley. (See “Nominate a Teacher for TMA’s Excellence in Science Teaching Awards,” page 36.)
“She was the one who told me that I could go to medical school, and it made a world of difference in my trajectory,” she said. “Now, she is my next-door neighbor. She got to see me become a physician, and I got the opportunity to pay her back by treating her students and our community.”
Dr. Escalona became a mentor herself as an assistant professor of pediatrics at UTRGV School of Medicine. The school, which opened to students just seven years ago, was the Rio Grande Valley’s solution to a lack of medical training in the area.
On the U.S. and Mexico border, rural areas in the Rio Grande Valley are among the most medically underserved areas in the country, per HRSA, with a lack of primary care physicians much like the case in Alpine.
What’s more, many schools in the area lack resources like fully equipped science labs or counselors knowledgeable about the medical school process.
To combat these deficiencies, UTRGV partnered with Region One Education Service Center to increase the number of health care professionals in the Rio Grande Valley. Region 1, part of a statewide system of education service centers, serves 38 school districts and 10 charter schools in eight South Texas counties, covering more than 400,000 students.
One major initiative between UTRGV and Region 1, the PATHWAY Conference in June 2019, provided eighth grade counselors and teachers from the 38 school districts knowledge, skills, and resources to give the proper career advice to aspiring health care professionals.
In addition to this initiative, UTRGV has created multiple community mentorship programs aimed at cultivating the next generation of physicians, and the school participates in JAMP. (See, “Paving the Way,” page 33.)
Alessandra Jimenez, a fourth-year medical student at UTRGV, says programs like these are crucial to connecting students with mentors who can “offer a seat at the table.”
“I was born and raised in the Rio Grande Valley, and my pipeline program for medicine began in middle school,” she said. “Had it not been for that type of exposure, I don’t know if I would have continued to pursue medicine the way I did.”
Once in medical school, Ms. Jimenez’s mentorship experience only increased.
“I can’t stress enough just how important it was that I had mentors through this process,” Ms. Jimenez said. “One of my mentors through medical school, [associate dean] Dr. Valdez, has personally guided me through decisions that I’ve made on what projects I should pursue and what specialties I’m interested in. It’s helped me tremendously.”
Despite UTRGV being less than a decade old, its resources have provided area students with knowledgeable role models within their own community, says Dr. Valdez, adding that she is honored to be a mentor herself.
Her experience gives her a way to support that community and connect with her students, many of whom have become beloved colleagues and friends.
“Mentees are almost like your kids,” she said. “I am so proud of my students and their incredible accomplishments.”
Nominate a Teacher for TMA’s Excellence in Science Teaching Awards
Each year, the Texas Medical Association’s (TMA's) Ernest and Sarah Butler Awards for Excellence in Science Teaching recognizes schoolteachers at the elementary, middle, and high school levels. These teachers’ energy and enthusiasm for science spark an interest within their students and often create medical professionals.
In 2014, TMA President-Elect Rick Snyder, MD, presented the award to his Dallas schoolteacher Janet Jones, who was his “inspiration.”
“She really triggered in me an interest in medicine and biology,” he said in a TMA video documenting the event.
Awardees are recognized in one of three ways:
• Grand Prize: One Texas science teacher receives $20,000 plus a $5,000 school resource grant.
• Distinguished Awards: Three teachers (one at each level) receive $7,000 and a $3,000 school resource grant.
• Rookie Award: A teacher with less than seven years’ experience receives $5,000 and a $2,000 school resource grant.
Texas full-time public and private school science teachers with at least two years’ completed classroom experience who are returning to a Texas classroom during the 2023-24 school year are eligible for this honor. Applications must include educational history and professional development, three letters of support, a professional essay, and a portfolio.
Physicians can nominate teachers by contacting Azalia Perez at azalia.perez@texmed.org. Applications open each summer.