
The Centers for Disease Control and Prevention (CDC) recently issued guidelines to help physicians prescribe opioids safely, and one of the reasons, the agency freely admits, is to clear up confusion caused by its last set of guidelines, which were issued in 2016.
It’s not that the 2016 guidelines were all bad, says Fredericksburg pain specialist and current Texas Pain Society (TPS) President Ralph Menard, MD.
He cites the case of a patient he inherited from another physician with a long history of neck and back surgeries. In 2016, the man had been taking the equivalent of 120 milligrams of morphine a day for several years. Because of a rigid adherence to the 2016 CDC guidelines, Medicaid would pay for only 60 milligrams a day.
For that patient, the change was fine. The new dosage kept the man’s pain under control.
But other pain patients forced to take lower dosages – or cut off from all medication – were not so lucky.
“There are reports of people committing suicide, or they went to illicit sources for pain medication,” Dr. Menard says.
The problem was that many people and organizations – lawmakers, insurance companies, pharmacies, physicians, and other health care professionals – misinterpreted or misused the 2016 guidelines, CDC says. As a result, pain patients nationwide faced arbitrary cutbacks on how much opioid pain medication they could receive.
Opioid prescriptions became difficult or impossible to obtain, even for patients with long-standing problems who had been stable on their medications, says Mesquite pain management specialist C.M. Schade, MD.
“There was a huge influx of patients [to my office] from primary care, from everywhere, because they couldn’t get any pain medicine,” said Dr. Schade, a former TPS president.
The 95-page 2022 CDC guidelines appear to be a big improvement on the 2016 version because they acknowledge past errors and don’t repeat those mistakes, Dr. Menard says.
“These are good recommendations,” he said. But, he added, the 2016 recommendations also were good for the most part. Physicians and other decision-makers in the health care industry now need to make sure they interpret these new guidelines correctly this time around.
Both sets of guidelines came in reaction to the “opioid crisis,” a period during the 1990s and early 2000s when opioids were widely overprescribed for pain, Dr. Schade says. In 2011, CDC branded prescription opioid use an “epidemic,” and new rules and awareness of the dangers of overprescribing began to cut the number of legal opioid prescriptions dramatically.
One of the biggest problems with the 2016 guidelines was that many in the medical community did not treat them as guidelines, Dr. Schade says. Since they came from CDC, they were wrongly treated as inflexible rules that applied to all physicians in all cases.
For instance, the 2016 guidelines gave recommendations about the “morphine milligram equivalent,” or strength of the medication, that is acceptable for primary care physicians to prescribe, says San Antonio anesthesiologist and pain medication expert Maxim Eckmann, MD, immediate past president of TPS. However, that guidance was not intended for subspecialists like pain physicians or oncologists who regularly treat pain.
“The guidelines became broadly interpreted as sort of reflective of the standard of care for all physicians treating pain and with relative inflexibility,” he said. “So certain states and stakeholders in states and medical boards started to enforce those limits, and payers did too. The Medicaid program and others enforced these limits as if they were a hard stop, and they were never really meant to be that way.”
In its new guidelines, CDC avoids recommending any specific dosages that could be similarly misinterpreted.
“In these recommendations, they don’t mention limits on anything,” Dr. Menard said.
However, CDC’s new document points out how the 2016 recommendations were misused.
For instance, CDC highlights the damage done by turning its recommended dosage guidance into rigid policy. Many states – including Texas – enacted laws limiting initial opioid prescriptions to 10 days or less. Also, insurers, pharmacy benefit managers, and pharmacies created similar policies, CDC says in the 2022 guidance.
Although these laws, regulations, and policies might have helped keep some people from overusing opioids, “they are inconsistent with a central tenet of the guideline: that the recommendations are voluntary and intended to be flexible to support, not supplant, individualized, patient-centered care,” CDC wrote.
That misapplication and inflexibility has, among other problems, forced patients to greatly cut back on or lose access to opioid-based medicines when they needed them, according to CDC. It also has caused cases of patient dismissal and abandonment.
“These actions … have contributed to patient harm, including untreated and undertreated pain, serious withdrawal symptoms, worsening pain outcomes, psychological distress, overdose, and suicidal ideation and behavior,” CDC said.
While opioid prescriptions nationwide have dropped by about 46% between 2012 and 2021, “drug-related overdose and death continue to increase, primarily due to illicitly manufactured fentanyl and fentanyl analogs,” according to the American Medical Association’s 2022 Overdose Epidemic Report. (See “Opioid Deaths vs. Opioid Prescriptions,” below.)
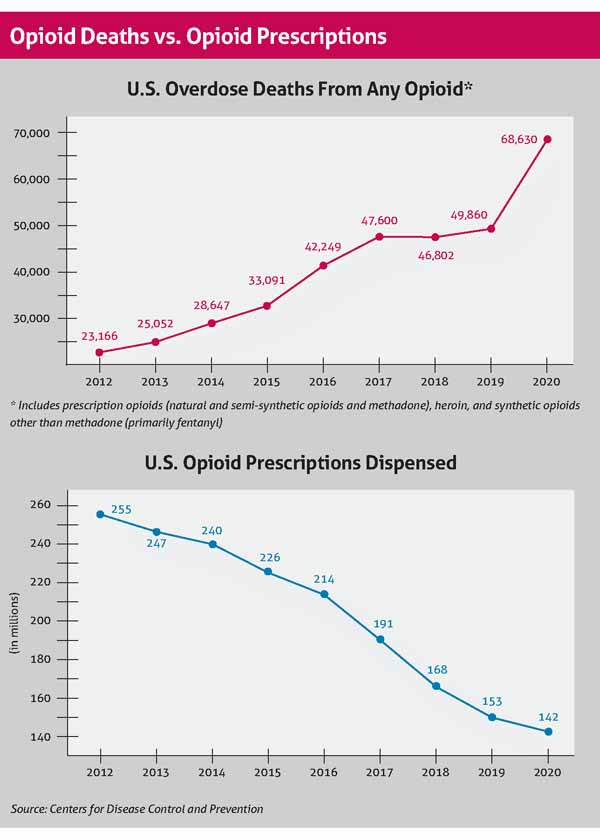
Overdose is one of the leading causes of death among adults 18 to 45 years old, and synthetic opioids like fentanyl are among the biggest causes of those deaths, according to CDC data. The number of 2020 overdose deaths involving synthetic opioids – most of them produced illegally – was more than 18 times the number in 2013, accounting for more than 56,000 overdose deaths in 2020.
Nevertheless, the backlash against the opioid epidemic makes pain medication difficult to obtain for many patients who need it, and physicians are part of the problem, Dr. Menard says. Some physicians refuse to prescribe opioids under any circumstances, and that prolongs their patients’ pain while kicking a treatable condition to other physicians.
Pain specialists must continue to individually educate family physicians, emergency physicians, and others in primary care that opioids are needed to treat pain.
“The problem is still based on those guidelines from 2016,” he said. “Many of those primary care doctors are still not prescribing any pain medication.”
The 2016 CDC guidance also has caused problems for patients and physicians among pharmacies, Dr. Eckmann says.
“There may be a case of a patient, for example, who’s been on a high dose [of an opioid-based pain medication] for years, and all of a sudden, the pharmacy says we’re not going to fill that medication anymore, even though the patient has been stable on it for years,” he said. “We’ve all heard about this problem, and it doesn’t seem to be going away yet.”
Most pharmacies do not cause this kind of difficulty for patients and physicians, he says. But TPS has received a steady stream of complaints from physicians who say this practice poses a significant problem for medical practices.
Large chain pharmacies – especially CVS, Walgreens, and Walmart – tend to present the most obstacles, while independent pharmacies seldom present problems, Dr. Eckmann says. The large chains have restrictive policies on filling opioid-based prescriptions, and in some cases employees interpret those policies as narrowly as possible, he says. (None of the three pharmacy chains replied to Texas Medicine’s requests for comment.)
When prescriptions are blocked or changed by the pharmacy, patients in need of pain relief frequently call Dr. Menard’s office in tears, triggering time-intensive chains of events for him and his staff, he says. A staff member must call the pharmacy to sort out why the prescription was not filled and coordinate between the pharmacy and patient. Moreover, Dr. Menard has to recheck the state’s prescription monitoring program database to reconfirm that the patient doesn’t have other opioid prescriptions that might interfere with his prescription.
“It just adds to the paperwork burden,” he said.
Health insurance policies complicate this picture by declining to pay for the physician’s choice of medication until the patient has tried other medications and not received adequate relief, Dr. Menard says.
Ultimately, the patient usually receives the medication he originally prescribed, but the process takes more time.
“We have to go through the litany of [medications] that the insurance company will allow,” he said. “The insurance companies ask [if] they’ve done these other medications – when did they do it, how long did they take it, and what was their effect. I’m working with [a mostly older adult] patient population that may not remember that.”
Requests like this frequently come from Medicare, but they’re common among other health insurance companies and occur in about 15% to 20% of Dr. Menard’s cases, he says.
Administrative pain relief
Physicians may see some relief from this problem thanks to House Bill 3459, which was approved by the Texas Legislature in 2021 with the Texas Medical Association’s strong support. It allows physicians to earn a “gold card” out of prior authorizations by demonstrating to insurers that they consistently earn approval for a particular service.
Also, in the past, many physician practices that prescribed opioids could be subject to a random inspection by the Texas Medical Board (TMB) to determine if the practice should be certified by the agency as a “pain management clinic.” If an entity is certified as a pain management clinic, it must comply with stringent administrative requirements, audits, and background checks.
Physicians reported to TMA that the fear of punitive regulation by TMB and the strict requirements for pain management clinics significantly interfered with access to patient care by deterring well-meaning physicians from prescribing valid, medically indicated pain medication.
In November 2022, TMB rewrote Rule 195.2, which now allows certain medical practices, including some certified pain management clinics, to qualify as a “gold-designated practice.” (Despite the similar name, it is not related to the gold card for prior authorizations.) The rule change allows physicians to submit proactively to a TMB audit to determine compliance with the law and then grants them a five-year grace period from additional TMB audits or investigations unless a specified triggering event occurs, such as a complaint or change of location.
The revision also allows primary care physicians to form partnerships more easily with psychiatrists, pain specialists, and other related health care professionals to provide patients with a multidisciplinary approach to pain management, says TMB President Sherif Zaafran, MD.
“Every [physician] as it stands can manage patients for chronic pain,” he said. “That has not changed. What has changed is incentivizing physicians to have a collaborative-type structure that we know is the best type of structure to manage chronic pain patients.”
Texas policymakers recently have embraced other efforts to reduce fentanyl-related deaths. For instance, Gov. Greg Abbott in December expressed support for legalizing fentanyl test strips, which help people identify whether look-alike medications contain fentanyl. While both the 2016 and the 2022 CDC guidance have rightly called for minimizing prescription opioid use, physicians find that difficult when it comes to prescribing nonopioid pain medications, Dr. Eckmann says. Payers often refuse to pay for those medications, even though they have been shown to provide greater pain relief than opioids and come with less danger of addiction.
“There are newer, more modernized pain medications that in certain populations may represent a better benefit and less risk,” he said. “They’re unfortunately quite expensive and not on [health insurance formularies].”
That problem has combined with a constant undersupply of opioid pain medications caused by supply disruptions. The shortage is part of a much larger shortage of many kinds of medications. But a March 2021 report published in PLOS One found that shortages of opioid analgesics are increasingly common, interfere with patient care, and increase health care costs.
“We’ve been caught between a rock and a hard place with less medication supply and fewer alternatives,” Dr. Eckmann said.