The Texas Medical Association’s reach extends far beyond the Lone Star State.
Take, for instance, a 2022 report by the Council on Socioeconomics that in part directed TMA to take a resolution to the American Medical Association advocating for a federal version of Texas’ new “gold card” law, which aims to curb onerous prior authorization practices by many state-regulated health plans and health maintenance organizations.
The TMA House of Delegates adopted the report at its annual meeting in Houston last April, referring the recommendation to the Texas Delegation to the AMA.
The delegation then worked to curry favor at AMA’s annual meeting in Chicago last June, where the AMA House of Delegates ultimately adopted Resolution 727, directing AMA to leverage its advocacy power to push for a federal version of Texas’ law.
Mark Casanova, MD, a palliative care physician in Dallas and an alternate delegate, says this is a good example of TMA’s leadership in AMA.
“It’s a combination of fortuitous timing coupled with a national need,” he told Texas Medicine. “These are not problems that just live in Texas. These are problems that affect damn near every physician in the country.”
TMA wields its influence in two ways: through the Texas delegation and through membership on AMA’s various councils and committees.
Like the TMA House of Delegates, the AMA House of Delegates is composed of scores of delegations, which represent state medical associations, national specialty societies, U.S. military branches, and AMA member groups. (See “Resolved: To Get Involved in Organized Medicine,” page 14.)
As part of the AMA house, Texas delegates hold voting authority on policy proposals that then inform national health care policy, federal agency rules, and industry best practices.
Also like TMA, Texas physicians serve on most of AMA’s councils and committees, where they help draft those proposals, on everything from scope creep to telehealth expansion to Medicare physician payment reform. (See “A Home Within TMA’s House of Delegates,” page 21.)
Fort Worth allergist and immunologist Susan Bailey, MD, has served as president of both TMA and AMA, giving her a unique perspective on how the organizations support each other.
“AMA and TMA work together on virtually almost any issue you can imagine because [they] are very supportive of the pluralistic payment system in medicine [and] supporting physicians’ ability to take care of their patients without interference from insurance companies and [other third parties],” she told Texas Medicine.
Dr. Bailey and other TMA member physicians involved in AMA leadership commend the Texas delegation, which they say is cohesive and effective. But they lament its size.
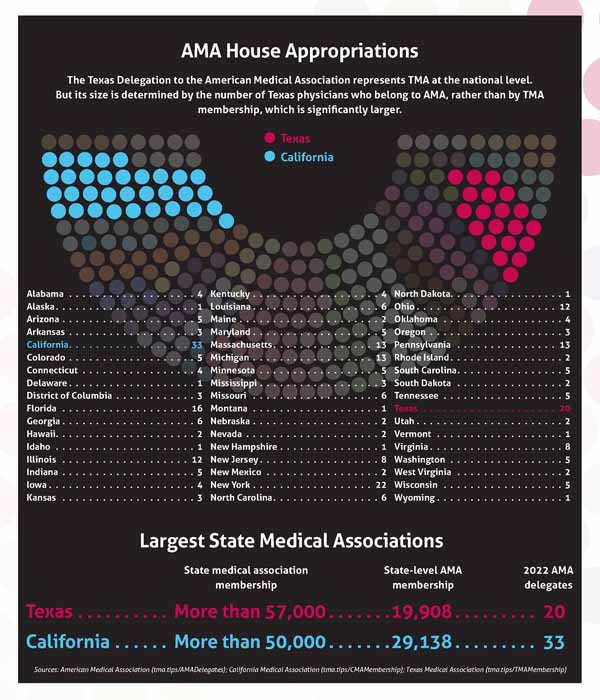
AMA bases its delegate count from each state on AMA membership, with roughly one delegate apportioned for every 1,000 AMA members. TMA is the largest state medical society in the country, with more than 57,000 members, but only about a third as many Texas physicians belong to AMA, which translates to a smaller delegation.
For this reason, Dr. Bailey encourages Texas physicians to join AMA, even if they disagree with some of its policies.
“It’s a proportional representation system,” she said. “So, the more AMA members we have [in Texas], the more influence we’ll have in the AMA House of Delegates.”
Maximum impact
TMA member physicians maximize their impact at the national level by serving on the Texas Delegation to the AMA.
AMA’s house is its principal policymaking body, made up of 600 voting delegates and 600 alternate delegates. Nearly 200 organizations help select delegates.
San Antonio pathologist David Henkes, MD, chairs the Texas delegation, which has 20 delegates and 16 alternate delegates.
“Our No. 1 responsibility and priority is to represent TMA and represent it well,” he said.
The AMA house meets twice a year, in June and November, for about five days each. The Texas delegation strategizes and prepares for these meetings at TMA’s annual TexMed, fall, and winter conferences.
TMA President and Texas Delegation Vice Chair Gary Floyd, MD, says this preparation frees up the delegation to focus on building relationships – and consensus – on the house floor.
For instance, the Texas delegation invites TMA member physicians from other state, national, and specialty delegations to caucus with it, amplifying its voice despite its relatively small size.
“The biggest thing has been [earning] the trust of other delegations in our Texas way of thinking,” Dr. Floyd said.
This strategy works.
After its success with the prior authorization resolution, the Texas delegation made a similar splash at the AMA interim meeting in Hawaii last November. Its members ensured AMA policy supported the continued use of telehealth beyond the pandemic, which is critical to Texas’ rural population, while addressing issues related to state medical licensure.
“In Texas, we really want to be sure that anyone who would be practicing has some accountability to the Texas Medical Board,” Dr. Henkes said.
Dr. Henkes says these wins would multiply with a more robust Texas delegation.
“Texas has the largest [state] medical association in the nation, but we don’t have the largest contingency to the AMA,” he said.
Although TMA’s physician membership outpaces that of the California Medical Association, at roughly 57,000 to 50,000, the Texas delegation is smaller than California’s, which has 33 delegates.
Dr. Henkes says this discrepancy means Texas has a weaker voice in deciding AMA policy than it could have. So, like Dr. Bailey, he urges TMA member physicians to join AMA, if they haven’t already.
“Whether any physician likes the AMA [or] doesn’t like the AMA, they need to understand that at the national level there is no one else,” he said. “We need to shape that voice, and the best way for us to do that is to have a large number of AMA members from Texas.”
AMA membership also brings with it fringe benefits, Dr. Bailey adds. For example, a major cause of burnout is a sense of helplessness, “of not being in control of what’s going on around you,” she said. “Being involved in health care policy and working with other physicians in other parts of the state or around the nation reminds us of why we went into medicine in the first place and how much more we have in common than we all realize.”
“A Texas viewpoint”
Dr. Bailey is a prime example of yet another way TMA physicians shape AMA’s voice: by holding elected leadership positions. That often starts with AMA’s various councils and committees, which surface policy proposals to AMA’s Board of Trustees and House of Delegates.
Tyler anesthesiologist Asa Lockhart, MD, has a long career in AMA leadership. He recently completed his term as chair of the AMA Council on Medical Service, where he brought what he called “a Texas viewpoint” to socioeconomic discussions.
“If I wasn’t there, then [the council] might [pursue] an option that might not be in political sync with most Texas physicians,” he said.
Sometimes, his advocacy resulted in an unmitigated victory, such as in the early 2010s, when he helped champion community-based care options for military veterans. He was motivated by seeing east Texas patients struggle to get timely appointments at the Veterans Affairs (VA) clinic in Tyler – or else struggle to keep appointments because they lived too far away.
AMA pushed Congress and then-President George W. Bush to offer community care options outside the VA system, with medicine ultimately endorsing the federal Veterans Access, Choice, and Accountability Act of 2014.
Other times, Dr. Lockhart has voiced opposition to a policy proposal, such as AMA’s support for the Affordable Care Act, or pressed for an alternative.
“You gotta be there to get a middle ground,” he said.
Dr. Bailey echoes this sentiment.
TMA’s role at AMA “has been not only to debate those policies that come out of those councils and press verbiage to improve them but also to get Texans on those councils so that our viewpoints are involved from the very beginning of the policymaking process,” she said.
Some AMA councils, such as the Council on Legislation, are appointed by the AMA Board of Trustees. But most are elected by the AMA House of Delegates.
Dr. Floyd, who also serves as vice chair of the AMA Council on Legislation, says a top priority of the Texas delegation is recruiting TMA member physicians to run for these leadership positions. To be eligible for such an office, physicians only must have been an active member of AMA for at least two years prior to election.
The Texas delegation’s strong reputation, burnished by TMA’s leadership on issues such as federal surprise billing legislation and state prior authorization reform legislation, has paid off with the recent elections of Dallas public health specialist John Carlo, MD, to the AMA Council on Science and Public Health, and of Lubbock critical care specialist Cynthia Jumper, MD, to the AMA Council on Medical Education.
Dr. Floyd also points to the 2022 interim meeting of the AMA house where TMA member physicians serving on AMA councils helped revise and avert several policy proposals that didn’t conform to TMA policy.
“If Texas speaks, people usually do listen to us,” he said.