Physician representatives of the Texas Medical Association last week took their expertise to an American Medical Association House of Delegates meeting punctuated this year by passionate discussions on scope of practice, health plan practices, COVID-19, telemedicine, diversity in medicine, and more.
Also at the Special Meeting held virtually June 11-16, AMA President Susan R. Bailey, MD, of Fort Worth concluded her presidency with sympathetic and inspiring words for her colleagues as she reflected on a year defined by the global COVID-19 pandemic.
The house installed its newest president, Gerald Harmon, MD, a family physician from South Carolina, and elected San Francisco dermatologist Jack Resneck Jr., MD, as president-elect to serve beginning in June 2022.
As house business got underway, Texas physicians once again were led successfully by Texas Delegation Chair David N. Henkes, MD, alongside TMA physicians active in several AMA leadership positions:
- San Antonio wound care specialist Jayesh Shah, MD, chaired the Reference Committee on Medical Practice and Facilities;
- Austin orthopedic surgeon David Teuscher, MD, chaired the Reference Committee on Legislation;
- Keller family physician Greg Fuller, MD, served as a member of the Reference committee on Medical Services;
- Tyler anesthesiologist Asa Lockhart, MD, chaired AMA’s Council on Medical Services; and
- Fort Worth pediatrician Gary Floyd, MD, served on AMA’s on Council on Legislation.
TMA continued work to ensure Texas maintains a strong voice in AMA. Dallas public health specialist John Carlo, MD, won his reelection to the Council on Science and Public Health; San Antonio radiologist Zeke Silva, MD, is a candidate for a seat on the Council on Medical Services in 2022; and Houston plastic surgeon Russell Kridel, MD, will run for AMA president for the 2023-24 term.
Bringing firsthand experience to the house – including a successful 2021 Texas legislative session – the Texas Delegation to the AMA was active through in-person and virtual testimony on a number of AMA policies to protect the profession of medicine and patients.
“We celebrated a year of superb AMA leadership,” said Dr. Henkes, a pathologist from San Antonio. “Although business was limited at this meeting to priority items of high importance due to the virtual format, over 64 resolutions and about as many AMA reports were examined and debated.”
The next AMA meeting in the fall is expected to be an in-person event.
Scope of practice
Texas physicians kicked off the meeting with early sponsorship of a resolution asking AMA to “actively oppose the American Academy of Physician Assistants’ recent move to change the official title of the profession from ‘physician assistant’ to ‘physician associate.’”
TMA and AMA had released earlier statements opposing the change.
Wholeheartedly adopting the policy, delegates acknowledged that physician assistants remain an important part of the health care team but expressed widespread concern that changing their name to “physician associates” will only confuse patients.
“In Texas we call this ‘Scope-A-Dope.’ And until we decide to take this bull by the horns, all they’re doing is confusing our patients. If you want to be a doctor, go to medical school,” Beaumont anesthesiologist Ray Callas, MD, said in speaking for the Texas delegation. He is a past chair of TMA’s Council on Legislation.
A similar proposal regarding confusion over the use of terms “residency” and “fellowship” in nonphysician graduate programs was referred for more study.
Private payer issues
Health plans’ use of prior authorization and discontinuation of nonphysicians’ ability to bill under a physician’s National Provider Identifier (known as “incident-to” billing) also garnered delegates’ attention with the house adopting new policies that come on the heels of TMA advocacy on similar issues in Texas.
Texas delegates supported the adoption of new AMA policies addressing peer-to-peer prior authorization that call for those approvals to be made actionable within 24 hours of the discussion, and to require that the reviewing physician have clinical expertise to treat the medical condition or disease under review. The latter policy is part of a landmark law TMA helped pass during the 2021 Texas legislative session.
“Particularly during a public health emergency like COVID-19, unnecessary prior authorizations should not stand between a patient and care they need," Dr. Bailey said in a statement.
Contending with Texas payers seeking to eliminate incident-to billing, the Texas delegation also supported adoption of a directive for AMA to advocate against such efforts among private and public payers.
On other coverage matters, TMA representatives were successful in encouraging more study of a proposal to lower the Medicare eligibility age from 65 to 60.
“While we support expanded access to care, this conflicts with physicians’ ability to provide that care,” Houston anesthesiologist Sherif Zaafran, MD, testified, citing several complex issues that require more analysis, such as costs.
Dr. Floyd also pointed to new provisions in the most recent federal COVID-19 relief package that address improved coverage for the uninsured.
Telemedicine
Acknowledging telehealth is not a replacement for in-person care, AMA, with Texas’ support, adopted a series of policies aimed at continuing the use of telehealth beyond the pandemic, while addressing issues related to state medical licensure, regulation, payment, and equitable access.
Lending his expertise as president of the Texas Medical Board, Dr. Zaafran testified to a number of “legal nuances” involved with a proposal for AMA to work with the Federation of State Medical Boards, state medical associations, and other stakeholders “to encourage states to allow an out-of-state physician to use telehealth to provide continuity of care to an existing patient in the state without penalty” if certain liability, HIPAA, and other conditions are met. The house referred the measure to the AMA Board of Trustees for a decision.
Texas also supported a resolution for AMA “to conduct or commission a study on the effects that telemedicine services have had on health insurance premiums, focusing on the differences between states that had telehealth payment parity provisions in effect prior to the pandemic versus those that did not,” and report back at AMA’s November 2021 Interim Meeting.
COVID-19 impacts
On other pandemic consequences, the AMA house voted to support the development of diagnostic codes to recognize post-acute sequelae of SARS-CoV-2 infection (“PASC 14” or “long COVID”) as a distinct diagnosis; advocate for legislation to provide funding for research, prevention, control, and treatment; and provide physicians and medical students with accurate and up-to-date information.
The house also voted to work with the Accreditation Council for Graduate Medical Education and other stakeholders to ensure residents and fellows whose training was interrupted by the pandemic, or who may have been redeployed to other specialty areas, get the support they need to qualify for graduation and board eligibility. The vote was a recognition of the impact of the pandemic on graduate medical education. The TMA House of Delegates enacted similar policy in May.
After long discussion, the AMA house referred for more study a separate education measure on ways to reduce financial burdens on trainees when it comes to covering costs for meals, uniforms, and child care.
Another long debate resulted in new, far-reaching AMA policy to increase diversity. With Texas’ support via online testimony, delegates adopted broad workplace guidelines that address systemic racism in medicine, including discrimination, bias, and abuse.
“AMA will recommend that health care organizations and systems use the new guidelines to establish institutional policies that promote positive cultural change and ensure a safe, discrimination-free work environment,” the organization said in a statement.
In other public health matters, as a result of a Texas resolution, delegates amended current AMA policy recognizing the negative physical and mental health effects of social media to advocate that those services include safeguards to protect vulnerable populations from harm.
“Adolescents’ and the general population’s reliance on social media has expanded,” as has the need for “evidence-based, reliable safeguards,” said Emily Briggs, MD, of New Braunfels, who testified in support of the measure on behalf of the American Academy of Family Physicians.
On other measures the Texas delegation monitored, the house voted to:
- Study and identify best practices for financially viable prospective payment insurance models;
- Oppose the practice of insurers providing financial incentives for patients to switch treatments and study its legality;
- Direct AMA to ask the Centers for Medicare & Medicaid Services to more tightly regulate Medicare Advantage plans so care is not limited;
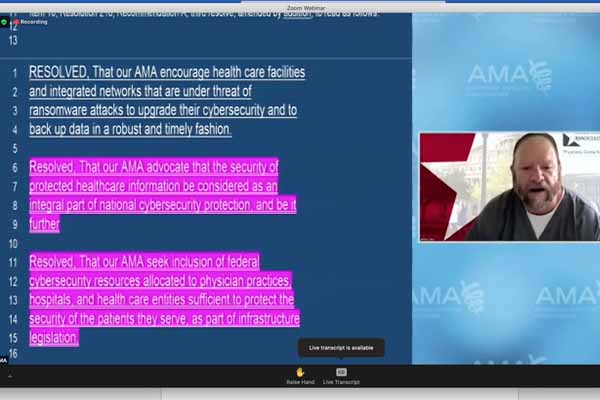
- Seek to introduce federal legislation providing for the prosecution of perpetrators of ransomware and any other malware on health care entities “to the fullest extent of the law”;
- Strongly advocate for legislation to allow borrowers to qualify for interest-free deferment on their student loans while serving in a medical or dental internship, residency, or fellowship program;
- Encourage the development of “clear, strong, universal, and enforceable” federal guidelines for the design and deployment of digital vaccination credentialing services that ensure accessibility, equity, and privacy, among other requirements;
- Urge national, state, and local health officials to “urgently assess the shortfall in funding, staffing, supplies, vaccine, drug, and data management capacity to prepare for and respond to a pandemic or other serious public health emergency”;
- Encourage design of personal protective equipment to better fit all body types;
- Investigate the Texas Coronavirus Antibody REsponse Survey project with the objective of implementing a similar program in other states or nationwide; and
- Oppose the use of drugs to chemically restrain agitated individuals outside of hospital settings for law enforcement purposes.