Physicians and other health care professionals should be vigilant to the possibility of monkeypox in patients after the Biden administration declared the outbreak a national public health emergency.
This advice stems from the Centers for Disease Control and Prevention (CDC), which began investigating its first confirmed case of monkeypox related to the current global outbreak that began in mid-May, and from the Texas Department of State Health Services (DSHS), which reports an uptick in new cases, about 300 as of this writing. The U.S. emergency declaration follows the World Health Organization's designation of the monkeypox outbreak as a global health emergency after tracking more than 16,000 cases in 75 countries and territories.
“If you feel like things are moving really quickly, that’s because they are,” DSHS Chief State Epidemiologist Jennifer Shuford, MD, said during a July 20 webinar held by the agency.
U.S. Department of Health and Human Services Secretary Xavier Becerra said the public health emergency declaration allows federal officials to "accelerate our response further" by freeing up funds and improving data-sharing.
Identifying monkeypox
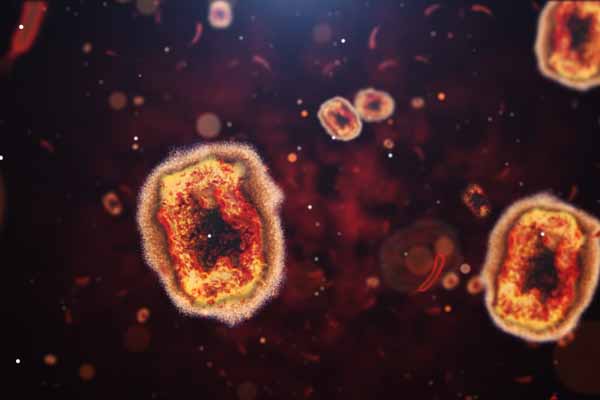
Monkeypox is a rare viral disease linked to the same family of viruses as smallpox, according to CDC. Monkeypox presents symptoms similar to smallpox – including a characteristic rash that may look like pimples or blisters accompanied by fever, headache, muscle aches, swollen lymph nodes, chills, and exhaustion – but is often milder and rarely fatal. It can spread through direct contact with infected people or animals, primarily through skin-to-skin contact.
The current global monkeypox outbreak is “really unusual” and poses challenges to physicians, many of whom have likely never seen a case of the disease, which is rarely seen in countries outside of Africa, said Trish Perl, MD, a member of the Texas Medical Association’s Committee on Infectious Diseases and chief of the infectious diseases division at UT Southwestern Medical Center in Dallas.
In suspected cases, physicians and other health care professionals should obtain specimens for testing, take patients’ sexual and travel histories, and notify their local health departments, according to CDC and DSHS.
Although early cases in the current outbreak were linked to social events in Europe and the U.S. largely attended by men who have sex with men, Dallas public health specialist John Carlo, MD, stresses that anyone can contract monkeypox.
“The reality is there’s nothing unique about the risk of monkeypox to people who identify as gay or men who have sex with men,” he said, adding that most Americans lack any protection against infection as routine smallpox vaccinations stopped in 1972.
Treating suspected cases
Detection isn’t the only challenge facing physicians amid the current outbreak. Dr. Perl says vaccines – which can help prevent monkeypox as pre- and post-exposure prophylaxes – and related treatments are in short supply, which is worrying given the speed with which new cases are being reported.
“Epidemiologically speaking … the concern is that we’re perhaps seeing the tip of the iceberg,” she said.
In response to the current outbreak, the U.S. Department of Health and Human Services has ordered nearly 7 million doses of Bavarian Nordic’s JYNNEOS vaccine, of which more than 300,000 doses have been distributed to states and jurisdictions, CDC reported during a July 26 webinar. The JYNNEOS vaccine was approved by the U.S. Food & Drug Administration in 2019 for the prevention of monkeypox and smallpox.
The American Medical Association recently approved new CPT codes for monkeypox testing and vaccination.
DSHS recently received a shipment of 14,780 doses of the JYNNEOS vaccine and forwarded 5,120 doses to Dallas County, which has reported the largest number of confirmed monkeypox cases in Texas. Houston and Harris County also received a separate shipment of approximately 5,000 doses.
DSHS does not expect to receive additional vaccine supply until late August or early September. Until then, the state agency says it will allocate doses to local health departments and its regional offices to vaccinate people with a documented or presumed exposure to monkeypox.
Texas physicians and health care professionals can place requests for the JYNNEOS vaccine through the state’s Vaccine Allocation & Ordering System.
There are no treatments for monkeypox, which typically lasts for two to four weeks. However, antiviral drugs developed to treat smallpox may be used to treat patients with monkeypox, especially if they are at high risk of severe illness, according to CDC.
Texas physicians can request antiviral treatments, including tecovirimat (also known as TPOXX), from their local health department for patients who have severe cases of monkeypox or who are at high risk of severe disease. DSHS will address such requests on a case-by-case basis, health officials said at the July 20 webinar.
Dr. Carlo, whose health center had treated roughly a dozen monkeypox patients as of late July, has struggled to access tecovirimat. He attributes the problem to short supply and to the drug’s “investigational use” status, meaning it is only approved for use in the context of a clinical study. As a result, Dr. Carlos says patients and physicians must sort through scores of pages of consent forms to participate in such studies.
More recently, CDC has updated this process to ease access to tecovirimat, including by reducing the number of patient visits and forms required, agency representatives said during the July 26 webinar.
Despite these issues, Dr. Carlo says all his monkeypox patients have recovered so far.
“Most people, thankfully, have just a few really bad days but are getting better pretty quickly,” he said.