
Insurance
Medicaid
Liability
Scope of Practice
Telemedicine
Public Health
Medical Education
PHYSICIAN-LED RESULTS
By Joey Berlin
AFTER MORE THAN four months of masking up, logging on, and clicking “send,” it all paid off handsomely.
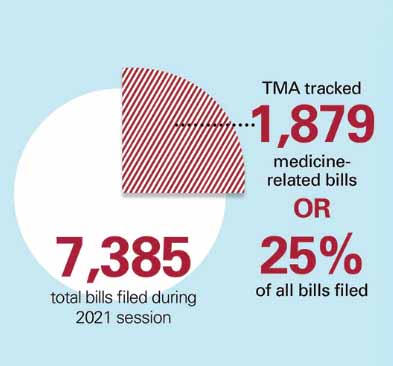
Texas physicians made the most of an extraordinary, scaled-back session of the Texas Legislature in 2021. With fewer floor meetings, no in-person First Tuesdays at the Capitol lobbying events, and limited air time for agenda items – made even more limited by the historic February winter storm – the House of Medicine needed its advocates to work harder than ever. Physicians needed initiative and drive to help get crucial legislation across the finish line – and help stop bad bills from becoming bad law.
They did all that with gusto. They helped pass laws to curb prior authorization hassles; keep physicians from incurring new practice costs; install liability protections for future pandemics like COVID-19; extend postpartum Medicaid coverage for new mothers; and keep graduate medical education (GME) fully funded. And so much more.
“Despite it being the most challenging year for doctors, we had more engagement than ever before leading to a very successful session,” said Austin oncologist Debra Patt, MD, who served as chair of the Texas Medical Association’s Council on Legislation during the 2021 session and testified 14 times at the Capitol.
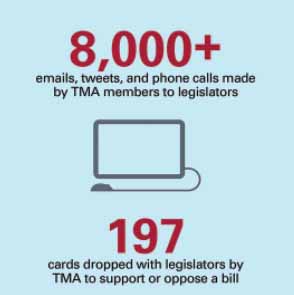
This year’s edition “posed unique challenges. But I will say there was a lot of grassroots advocacy,” she said. “TMA quickly pivoted to Zoom, virtual outreach, and a lot of TMA members attended virtual meetings with their legislators.”
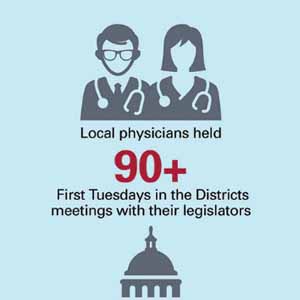
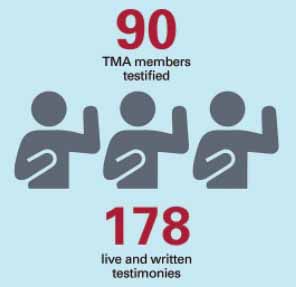
Nearly 90 TMA members testified for the House of Medicine during the session, and members responded in droves to urgent alerts TMA sent out urging action on specific measures like scope-of-practice bills. Appropriately, the result was a pandemic-era shot in the arm for Texas health care that doesn’t cure all, but will leave lasting positive impacts inside the system. Here’s an overview followed by specifics you can read about in the articles on the following pages.
Early win, strong finish
Medicine scored the very first piece of law to result from the 2021 session when Gov. Greg Abbott signed a measure eliminating an upcoming tax on outsourced medical billing services.
Advancement on key measures slowed after that, but a furious final few days produced a slew of other wins. A measure allowing physicians to earn a “gold card” out of the prior authorization process – and requiring peer-to-peer calls for utilization reviews to be conducted by a Texas-licensed physician in the same or similar specialty – survived to become law despite dogged insurer opposition. Insurer transparency will be enhanced thanks to a bill providing for an all-payer claims database.
In Medicaid, TMA shot for one year of postpartum coverage for women who give birth, but settled for six months – a four-month improvement on the status quo. Children in Medicaid now will have the opportunity for two continuous six-month periods of coverage, contingent on a household eligibility check near the end of the first six-month period.
Pharmacy benefit managers will no longer be able to “claw back” millions of dollars in “direct and indirect remuneration fees” from Texas practices; a bill to outlaw those fees passed thanks to TMA advocacy. Telemedicine, having proved its immeasurable value during the pandemic, got a boost with permanent relaxation of certain Medicaid restrictions on its use, as well as a measure aimed at improving the state’s broadband capabilities. Public health wins for the House of Medicine included a licensure requirement for e-cigarette dealers – helping establish a framework to tax vaping products in the same manner as tobacco products – and measures that help ensure the state’s personal protective equipment and improve public health reporting for the next disaster.
Budget success and a look ahead
Throughout the session, TMA was adamant that the state’s GME grant program continue to be fully funded in the state budget to maintain the 1.1-to-1 ratio of residency slots per medical school graduate. The legislature listened, allocating the full $199.1 million that medicine was asking for over the next two years. Other wins included a slight increase in women’s health funding ($352.6 million overall), level funding for early childhood intervention services ($339 million), and nearly $20 million more for the Texas Mental Health Care Consortium ($339 million).
Houston emergency physician Diana Fite, MD, TMA’s president for the majority of the session, notes medicine had to fight to successfully avoid cuts for health care services because in the midst of the pandemic in 2020, Governor Abbott asked many state agencies to cut their then-current budgets by 5%. She says the expectation was that when lawmakers constructed the 2022-23 budget, further cuts would be in store.
“In some of those items to actually get a little more money coming in was a win,” said Dr. Fite, who testified four times for medicine.
On the other hand, TMA’s push for some form of coverage expansion for uninsured Texans and its perennial pursuit of physician payment increases in Medicaid went unrealized, although the state will conduct a study on the cost-effectiveness of a pay bump for pediatric Medicaid care.
John Carlo, MD, a seven-time testifier during this session, says the budget was ultimately a mixed bag.
“We got some things we needed, but we were missing some other things that we really would like to have seen happen,” he said, adding that budget writers could have paid more attention to the state’s pandemic response. “I think we want to see continued support of our laboratories. What we’ve learned is that there’s still some need for stronger public health infrastructure.”
The House of Medicine’s work won’t be done this year. At press time, one special session had begun and another was expected, with one task for the legislature being to mete out $16 billion in federal COVID-19 aid. TMA will push for those funds to be allocated in a way that’s beneficial for the health of Texans.
INSURANCE: Medicine earns its gold star
By Joey Berlin
When it came to addressing prior authorization burdens this legislative session, the Texas Medical Association asked physicians directly what they needed, and those responses helped medicine attack the problem with a laser-like focus.
In one of TMA’s most gigantic wins in the insurance realm, and in the entire 2021 session, Texas physicians will soon be able to earn a “gold card” exempting them from the preauthorization roadblocks of state-regulated health plans. And the Texas bill is quickly becoming a model for other states.
Under House Bill 3459 by Rep. Greg Bonnen, MD (R-Friendswood), physicians can earn a continuous gold card by earning approvals on at least 90% of their preauthorizations on a given service over a six-month period.
“There’s no question that the gold-carding item will be very helpful for physicians to save a massive amount of time for them and for their office staff in not having to get prior authorizations on so many things, every single day and every single week,” said Houston emergency physician Diana Fite, MD, TMA’s president through mid-May 2021. “That will help not only the physicians and their office staff, but help immensely [patients’ ability] to get the care that they need in a timely fashion, and not have them sometimes give up on getting the care because of the frustration of the delays.”
The ability for physicians to effectively test out of prior authorization could be an enormous administrative boon for doctors like internist Lisa Ehrlich, MD, who testified for TMA on behalf of HB 3459 during this session. She says in the past five years, health plans have required prior authorizations “across the board” for just about everything. She’s collected years of aggravating anecdotes involving health plans delaying and denying care through preauthorization.
One that sticks out to her: a patient who had appendicitis on the eve of a major storm’s arrival. The patient got a CT scan at the hospital, then headed to the emergency department for surgery, where she waited 12 hours for her prior authorization to come through. Her appendix ruptured in the waiting room, and she ended up having to stay in the hospital during the storm, plus an additional two weeks.
“Acute appendicitis is not that hard to diagnose; [it’s] pretty easy,” Dr. Ehrlich said. “Basically, the insurance companies are getting in the way saying, ‘OK, you have to prove to us the patient has appendicitis at first through the CT scan, and then you have to prove he needs a CT scan to prove that they have appendicitis. Then it just goes on and on. Virtually right now everything is requiring prior authorization.”
Although the gold card will be continuous after it’s initially granted, health plans will have the opportunity to reevaluate physicians’ status up to twice each year and must notify the physician at least 25 days before a rescission would take effect, with the physician getting a chance to appeal to an independent review organization.
But HB 3459 didn’t just allow physicians a needed path out of the preauthorization rigmarole. It also included language representing something that’s become a white whale for medicine: making sure physicians who conduct peer-to-peer calls for insurers’ utilization reviews are (1) licensed in Texas, and (2) know what they’re talking about.
The new law requires peer-to-peer calls occurring prior to a utilization review denial to be conducted by a Texas-licensed physician in the same or similar specialty as the physician who requested the service. That means no more trying to explain the appropriateness of a procedure to some out-of-state physician in an unrelated subspecialty.
It was physicians who helped make that crucial piece of the bill happen by responding to lawmakers through TMA’s Grassroots Action Center.
“Does it seem right that an OB-Gyn specialist from Maryland can tell a board-certified neurosurgeon in Texas with over 22 years of experience that an MRI scan of the cervical spine for a patient with arm pain, numbness, and weakness is not necessary?” one neurosurgeon rhetorically asked in an Action Center message to a lawmaker. “I will have to change my practice patterns if there is no relief from prior-authorization hassles, which will mean less care for Texans.”
TMA lobbyist Clayton Stewart says both the gold-card and the utilization review pieces of the bill have real potential to lessen prior authorization burdens “because the concepts in the bill were taken from our physician-members – what they said would be helpful to them, help them get their patients the care they need when they need it.”
While Representative Bonnen carried the ball for HB 3459 in the House, another physician lawmaker, Sen. Dawn Buckingham, MD (R-Lakeway), spearheaded the bill’s advance in the upper chamber.
Bill me never: Tax averted, and other wins
Meanwhile, TMA also scored a major insurance win with the first bill Gov. Greg Abbott signed during this year’s session, which declassified medical billing services as insurance services.
That simple designation in landmark House Bill 1445 by Rep. Tom Oliverson, MD (R-Cypress), meant that outsourced medical billing services won’t be subject to a tax that was slated to take effect in October. Medical billing companies would have passed the added costs onto physicians, and patients would have seen a ripple effect reach their wallets as well.
Comptroller Glenn Hegar had previously examined state insurance law and decided in 2019 that medical billing services were considered insurance claims processing. Originally, the medical billing tax was set to go into effect on Jan. 1, 2020, but advocacy from TMA helped win two delays, pushing back implementation until after this year’s session. That gave TMA, with the comptroller’s help, a chance to craft a legislative fix.
“This is an example of good advocacy. The only reason this happened is because ... TMA reached out to me before session, explained the problem to me,” Representative Oliverson told Texas Medicine. He said he called the comptroller and was able to “explain our side and why this was really problematic for smaller practices that don’t have their own in-house billing company. [The comptroller] was very willing for us to fix it legislatively. None of that would’ve happened, though, without TMA advocacy.”
Other medicine-supported insurance wins from this session include:
• In an effort to increase payer transparency, House Bill 2090 by Rep. Dustin Burrows (R-Lubbock) authorizes the creation of an all-payer claims database through the Center for Healthcare Data at UTHealth in Houston. The database will include claims data, contracted rates, and other information.
• Senate Bill 827 by Sen. Lois Kolkhorst (R-Brenham) generally caps patient cost-sharing for prescription insulin at $25 per prescription for a 30-day supply.
• Senate Bill 1028 by Sen. Joan Huffman (R-Houston) lowers the minimum age at which health plans are required to cover colorectal cancer screenings to 45, instead of 50.
• Senate Bill 1065 by Sen. Carol Alvarado (D-Houston) requires health plans to cover screenings for dense breast tissue at the same level as mammography.
MEDICAID: A big step forward for maternal health
By Sean Price
One of the Texas Medical Association’s biggest wins this session came in the partial realization of medicine’s longtime advocacy to extend Medicaid coverage for postpartum maternal care.
House Bill 133, authored by Toni Rose (D-Dallas) and sponsored by Sen. Lois Kolkhorst (R-Brenham) in the Senate, provides women enrolled in pregnancy-related Medicaid with six months of postpartum coverage, an increase from the two months they currently have.
“We very much appreciate all the work that [Rep.] Toni Rose as well as Sen. Lois Kolkhorst did for us in getting those extra four months,” said New Braunfels family physician Emily Briggs, MD, who sits on TMA’s Committee on Reproductive, Women’s, and Perinatal Health.
TMA strongly supported obtaining 12 months of coverage in this session, but getting the coverage level up to six months was still a “great start,” says Kimberly Carter, MD, an Austin obstetrician-gynecologist and co-chair of TMA’s Task Force on Health Care Coverage. The task force, made up from a cross-section of Texas physicians, was created in March to provide data and feedback on legislation designed to extend Medicaid coverage and – more long-term – to guide policymakers on all efforts that expand access and care.
“We are moving in the right direction and are really excited that the legislators prioritized this issue to successfully pass an extension, but we continue to have a goal of 12 months,” she said.
Obtaining 12 months of coverage remains an important target for future Texas legislative sessions because medical evidence shows that women run into a wide variety of medical problems in the year after giving birth, Dr. Briggs says.
In March, she wrote to the House Appropriations Committee on behalf of TMA and other medical groups that “too many women die during pregnancy or in the year following, though nine in 10 of these deaths were potentially preventable.”
Many women who have important problems like postpartum depression, hypertension, and other morbidities common after delivering a baby are not diagnosed until several months after the birth, says Dallas public health physician John Carlo, MD. They often have to wait weeks or months to begin care with the appropriate specialist, and by that time even a six-month Medicaid benefit will have run out.
“It’s a victory, but it’s a guarded one because I really wonder if we have the networks of [physicians], especially around psychiatry and behavioral health and cardiovascular diseases and the things we know cause the morbidities after pregnancy,” he said.
Even when women are able to obtain treatment, postpartum health problems often require lengthy treatment, Dr. Briggs says.
“When [a woman is] first being treated for, say, hypertension, it’s not like we give her medicine and she’s cured,” she said. “We need time with that medication for lifestyle management or for coping mechanisms if its depression. … It’s an ongoing life issue. It’s not like a gallbladder being removed and, blam, you’re done.”
Despite these drawbacks, extending Medicaid coverage to six months is a substantial improvement and will benefit Texas women as well as their families, Dr. Briggs says.
“When you’re providing care to mom, you’re elevating care … to the entire family,” she said. “You’re encouraging that mom to find a medical home. You’re encouraging her to have a place to go when her partner has an issue, when her child has an issue, when the rest of the family needs care. So, you’re benefiting the community by benefiting the mom’s access to care. I think that’s a big reason that this is such a big win.”
Other legislative highlights in maternal care include:
• A $5.6 million increase for women’s health services – including Healthy Texas Women, the Family Planning Program, and Breast and Cervical Cancer Services – compared with the 2020-21 biennium.
• $47 million allocated in general revenue to implement six months’ postpartum Medicaid coverage.
• $7 million to continue TexasAIM, a statewide maternal safety initiative, and to develop and establish a high-risk maternal care coordination services pilot for women of child-bearing age.
Extended coverage for kids
The Texas Legislature also approved House Bill 2658, which among other provisions provides children under 19 years old on Medicaid with two consecutive six-month periods of coverage. The measure, which started off as House Bill 290 by Rep. Philip Cortez (D-San Antonio), was amended onto HB 2658 to improve its chances of passage.
As filed, HB 290 would have provided children on Medicaid with 12 months of continuous coverage, a proposal called for by TMA. Instead, the compromise language directs Texas Medicaid to provide children six months of continuous coverage followed by one electronic income verification at six months. Children confirmed eligible will retain coverage for another six months. However, if the electronic income check cannot confirm eligibility, which is often the case, parents will be given 30 days to provide documentation, up from just 10 days currently.
Families with children on Medicaid have been forced to regularly prove their child is eligible for Medicaid services, and this new law eases that burden, Dr. Briggs says.
“There was a lot of bureaucracy, a lot of red tape that resulted in a lot of kiddos losing their coverage, and this House bill essentially removes [most of] that red tape,” she said. “It makes it so that children can continue their coverage without having to jump through so many hoops.”
HB 2658 also provides payment for one preventive dental care exam for adults with disabilities who are in the Star+Plus Medicaid managed care program. That is a major step forward for public health as well because it will help prevent more serious dental problems later – problems that contribute to poorer health and higher use of emergency departments, says Helen Kent Davis, TMA’s associate vice president of governmental affairs.
Despite these successes, Texans’ access to Medicaid remains limited overall. Legislators declined to pass a plan to accept federal Medicaid funds, which would have extended health care coverage to 1 million more Texans than are currently covered, Dr. Carter says. Physicians need to push lawmakers to come up with a Texas solution to improve access to care for more people, she says.
“One of our reasons for increasing [physician Medicaid payments] is that it is linked to increased access to care,” Dr. Carter said. “There are doctors who say they don’t want to take those patients because [Medicaid] doesn’t pay enough.”
Dr. Briggs in her March testimony pointed out that Texas has not enacted a meaningful, enduring physician rate increase in more than a decade.
LIABILITY PROTECTIONS: Assurances for the next pandemic
By Joey Berlin
Physicians inherently want to help people – that’s why they’re physicians. But as COVID-19 has shown, there may be no harder situation in which to help Texans than during the rigors and pressures of a pandemic.
So physicians in that situation need assurances – specifically, liability protections that account for the extraordinary situation they’re in. Senate Bill 6 by Sen. Kelly Hancock (R-North Richland Hills), passed with organized medicine’s support, provides some of that.
“Having better liability protections during the pandemic just helps to protect medicine to act in the public’s best interest to the best degree that we can,” said Austin oncologist Debra Patt, MD, who was chair of the Texas Medical Association’s Council on Legislation during most of this year’s legislative session. “So it’s important in our early response and participation in future emergencies.”
SB 6 specifically provides some liability protection for physicians (as well as other practitioners, health care institutions, and first responders) during a pandemic if certain conditions are met. The bill generally relieves them of liability for injury or death caused by (1) providing care or treatment to a person during a pandemic, or (2) lack of care or treatment – regardless of the circumstances under which the person was injured or died. If sued for such an event, physicians may avoid liability by proving by a preponderance of evidence that:
• The pandemic disease was a cause of the care or treatment, or lack thereof, that caused the injury or death; or
• The person who was injured or died was “diagnosed or reasonably suspected to be infected with a pandemic disease” at the time.
The bill doesn’t protect reckless conduct or intentional, willful, or wanton misconduct. Otherwise, protected care or treatment under SB 6 includes:
• Screening, assessing, diagnosing, or treating someone who’s infected with the pandemic disease or is suspected of being infected;
• Prescribing, administering, or dispensing a drug for off-label or investigational use to treat such a person;
• Diagnosing or treating a pandemic disease outside the physician’s normal specialty area;
• Delaying or canceling nonurgent or elective procedures, as well as delaying, canceling, or not accepting in-person appointments for pandemic-unrelated illnesses; and
• Acts or omissions caused by a lack of staffing, facilities, supplies, and other resources attributable to the pandemic.
“That’ll definitely help us this time and with the future, because there’s just no way that you can know at the onset of a pandemic on a new disease, what to do with it,” said Houston emergency physician and TMA Immediate Past President Diana Fite, MD. “You treat it the best you can.”
The law covers pandemics and disaster declarations related to pandemics but doesn’t provide new protections related to hurricanes or other natural disasters. Importantly, it contains several deadlines that limit when physicians can exercise the new protection if a lawsuit is filed. A physician may mount his or her defense under the law no later than the latest of these three dates:
• 60 days after SB 6 went into effect on June 14, 2021, which is particularly important for a suit that was already filed;
• 120 days after the physician files an answer to the lawsuit; or
• 60 days after the person suing serves an expert report on the physician.
Dallas public health physician John Carlo, MD, says SB 6’s provisions covering not only care, but also failure to provide care, are particularly important for when “we’re in a situation where we’re having to change everything from scheduled procedures, or having to change what we traditionally do.”
SB 6 was a collaboration between the Texas Civil Justice League and other business and professional organizations. Medicine enthusiastically backed the bill.
“It is a comprehensive bill that covers liability protections during a pandemic for broad swaths of Texas business, including health care,” said Dan Finch, TMA’s vice president of advocacy. “We’re grateful to have been part of a team effort to support it.”
Other existing liability protections also may protect physicians in these types of cases. For some examples, consult a TMA white paper available free to members at tma.tips/volunteerliability.
BAD IDEAS, GOOD RESULTS: Medicine’s voice helps kill dangerous scope bills, other ill-advised legislation
By Joey Berlin
Once again, expertise prevailed in this year’s legislative session. So did good sense.
The 2021 roster of anti-medicine ideas put forth in legislation at the Capitol may have looked familiar. For instance, nonphysician practitioners put forth their usual patient-endangering attempts to expand their scope of practice into medicine: independent prescribing for nurse practitioners, optometrists performing surgeries, psychologists prescribing drugs, and more. But the Texas Medical Association helped stop each of those scope proposals well short of becoming law, once again convincing lawmakers that physicians should be the leaders in a collaborative care team effort with other practitioners.
The House of Medicine also helped kill several pieces of anti-vaccination legislation and bad ideas on advance directives and end-of-life care, among others.
Productive comprom-eyes
As for an optometry bill that turned out to be the biggest scope threat, medicine successfully mitigated its dangers through a mutually beneficial compromise.
As originally filed, Senate Bill 993 by Sen. Kelly Hancock (R-North Richland Hills) would have allowed optometrists to perform a number of different kinds of eye surgeries.
The curriculum in Texas’ optometry schools “have some anatomy and physiology of the eye, not the rest of the body. They have minimal pharmacology training,” says Mark Mazow, MD, president of the Texas Ophthalmological Association (TOA) and a testifier against the bill on TOA’s behalf during this session. “Using medicines and interacting with the rest of the body is not nearly at the level in any way, shape, or form as a medical doctor or [osteopathic doctor]. And they have no surgical training. … The rest of their education does not prepare them for the complications or risks that accompany all surgical procedures.”
As part of a substitute for the original bill, the compromise between TOA and organized optometry stripped out the surgery language, instead creating an ophthalmologist-involved peer review process for glaucoma complaints lodged with the Texas Optometry Board. In exchange, optometrists gained authority to manage mild-to-moderate glaucoma without having to co-manage the condition with an ophthalmologist, and expansion of their ability to administer topical and oral medications for the eye. After the deal was struck, SB 993 suddenly became a measure TMA could support, and it passed without issue.
Sen. Dawn Buckingham, MD (R-Lakeway), an ophthalmologist and an instrumental player in the compromise legislation, said the key was its collaborative peer-review panel that involves both ophthalmologists and optometrists.
“The whole goal is that when a patient [receives] care, they should expect that same standard of care regardless of the provider that they seek,” Senator Buckingham said. “That way, optometrists and ophthalmologists will be held to the same standard.”
Dangerous prescriptive authority
Meanwhile, no compromise was needed to bury other bad scope measures.
House Bill 2029 by Rep. Stephanie Klick (R-Fort Worth), which would have granted advanced practice registered nurses independent prescribing authority and other haphazard autonomy, didn’t pass. Neither did House Bill 1462 by Rep. Vikki Goodwin (D-Austin), which would have allowed psychologists to prescribe drugs.
Fort Worth child and adolescent psychiatrist Debra Atkisson, MD, has personal experience illustrating why psychologists aren’t qualified to prescribe.
She told Texas Medicine she examined a boy referred by a psychologist who “knew” the boy had ADHD and needed Ritalin. But she noticed “some things with his eye movement, and I also noticed that in some ways, his motor skills on one side were a little different. And I thought, ‘I think this could be neurological,’” Dr. Atkisson said.
“To make a long story short, he had a brain tumor. What the child neurologist said to me was, ‘If you had prescribed the Ritalin, he would’ve probably had a seizure on that. Then we would’ve found the brain tumor after he fell on his head, which probably wouldn’t have been good,’” she said. “The child actually did all right. But the bottom line is, it’s because I was trained as a medical doctor that I was able to determine, ‘This is probably not just ADHD.’”
Also on the medication front, medicine’s advocates stopped Senate Bill 735 by Sen. Angela Paxton (R-McKinney), which would have allowed midwives to administer drugs “commonly used in labor or postpartum care” without a physician’s involvement.
Recently retired Austin obstetrician-gynecologist Diana Weihs, MD, believes the drug midwives probably had most in mind was oxytocin, known by the brand name Pitocin. She says the drug, used to help the uterus contract and decrease bleeding, has a reputation for being one of the most dangerous drugs in obstetrics. Dr. Weihs testified against the bill during this session on behalf of the Texas Association of Obstetricians and Gynecologists, as well as the American College of Obstetricians and Gynecologists.
“There were no stipulations about where they would be using it – in a birthing center, or at home. There would be no physician aware of the patient or prescribing the drug,” Dr. Weihs said. “Postpartum hemorrhage is one of the leading causes of maternal mortality. It is crucial to have physician backup in those situations.”
Pharmacists also tried to advance into the practice of medicine but without success. Other defeated scope-of-practice bills included House Bill 678 by Rep. Philip Cortez (D-San Antonio) to allow pharmacists to order immunizations and vaccinations on patients aged 3 and up, and House Bill 2049 by Rep. Donna Howard (D-Austin) to allow pharmacists to test and treat strep throat and the flu.
Anti-vax, end-of-life bills defeated
Anti-vaccination bills were also as prevalent as ever during this session, but medicine worked tirelessly and successfully to defeat them all, along with other bad legislation. Those measures included Senate bills 1310, 1313, and 1669, all by Sen. Bob Hall (R-Edgewood):
• SB 1669, billed as a measure to bar anyone from discriminating against someone based on vaccine status, would have removed all existing Texas vaccination requirements.
• SB 1310 would have required physicians to give parents information on vaccine excipients to obtain informed consent to immuize their child.
• SB 1313 would have allowed people to not participate in a host of infection control measures and created barriers to implementing those measures when needed.
On the end-of-life front:
• House Bill 2180 by Rep. Joe Moody (D-El Paso) would have allowed for multiple people to simultaneously become “co-agents” with medical power of attorney on another person’s behalf.
• Senate Bill 917 by Sen. Bryan Hughes (R-Tyler) would have forced physicians to treat an end-of-life patient indefinitely until a transfer facility could be found, even if the physician believed the treatment was medically inappropriate and the facility’s ethics committee agreed.
TELEMEDICINE: Steps forward in Medicaid, broadband
By Joey Berlin
Coming into the 2021 session, the Texas Medical Association had hope that telemedicine’s success in allowing for remote care during the COVID-19 pandemic would prompt lawmakers to permanently relax many state policies restricting its use.
That didn’t happen to the degree that TMA wanted. But with the House of Medicine’s urging, the legislature did advance telemedicine in some important ways, demonstrating an understanding of how valuable remote care can be.
During the early days of the pandemic, telemedicine’s acceleration was made possible by the temporary easing of state and federal restrictions, including in Medicaid. House Bill 4 by Rep. Four Price (R-Amarillo) helps keep telemedicine on the right path by making some of those changes in Medicaid permanent.
The bill requires the state to ensure that Medicaid and Children’s Health Insurance Program patients, among others, “have the option to receive services as telemedicine medical services, telehealth services, or otherwise using telecommunications or information technology,” with consideration of federal law and whether such services are clinically appropriate and cost-effective. Services listed in the bill include those for preventive health and wellness, case management, behavioral health, and nutritional counseling.
The bill also opens the door for continued use of audio-only services and physician payments for delivering home telemonitoring services.
“This was an agreeable allowance for a particularly vulnerable subset of Texas patients,” said Austin psychiatrist Thomas Kim, MD, an active advocate for telemedicine who testified for TMA on the topic at both the state and congressional levels during this session.
“Of all places to go, [the Medicaid program is] a great place to start,” he said. “These are the folks that typically struggle with social determinants of health more, and as a result, struggle with health and wellness.”
The legislature also aimed to take care of the technical side of telemedicine – specifically, the lack of broadband access in many areas – with House Bill 5 by Rep. Trent Ashby (R-Lufkin). HB 5 establishes a state broadband development office, which will create a program to award financial incentives, including grants and low-interest loans, to applicants (such as companies) that can help expand broadband in areas particularly lacking it.
Also encouraging for telemedicine’s continued advancement, the state’s budget included a rider that directs the Texas Health and Human Services Commission to pursue increased use of telemedicine and telehealth in Medicaid as a way to curb costs. (Although the two terms are often used interchangeably, under Texas law telehealth is the remote delivery of health care services other than telemedicine, while telemedicine specifically refers to remote health care services delivered by a physician, or under a physician’s delegation and supervision.)
For both physicians who’ve known telemedicine’s upside for a long time and those pleasantly surprised after being pushed into it by the pandemic, these steps are welcome news.
“I am amazed at how I have been able to see high-functioning autistic kids in a residential treatment center and develop a rapport and bond with them using telepsychiatry, and treat them,” said Fort Worth child psychiatrist Debra Atkisson, MD. “This has really freed psychiatrists to be able to expand and see more people in more places.”
Yet another measure related to physician licensing also could help those wanting to practice telemedicine. House Bill 1616 by Greg Bonnen, MD (R-Friendswood), authorizes Texas to participate in the interstate medical licensure compact, along with 29 other states, which could facilitate licensing for physicians new to Texas and Texas physicians who want a license in more than one state. The expedited licensing process is voluntary, and at least 80% of applicants for Texas medical licenses are estimated to be eligible.
Payment parity put off
However, one of medicine’s most important asks in the telemedicine realm – permanent payment parity for those services – didn’t get through this year.
House Bill 980 by Rep. Art Fierro (D-El Paso) would have required insurers to pay for a covered service delivered via telemedicine “at least at the same rate” as for an in-person service. It never reached the House floor.
The bill would have codified TMA’s long-standing position on telemedicine payments: As long as physicians meet the standard of care in providing a covered service, whether they delivered the service in person or via telemedicine should make no difference with regard to payments. If that’s not the case, telemedicine simply isn’t worth it to many physicians.
“To have a disparate payment structure only serves to continue to inhibit or limit telehealth’s continued growth or maturation as a critical and very useful tool that all physicians should take advantage of,” said Dr. Kim, who testified before the Texas House Insurance Committee in support of HB 980. He hopes convincing lawmakers to go for payment parity in future sessions isn’t a matter of proving telemedicine’s care value and cost-effectiveness.
“I know that there are still people who persist in that narrative. I think as far as demonstrating the value, you only have to look at the history of just this last year,” he said.
Diana Fite, MD, TMA’s president during the bulk of the session, says just highlighting the broadband deficiencies in rural areas made this session helpful on the telemedicine front, and she isn’t totally discouraged by the payment parity measure not passing.
“Some insurance companies may still pay equal to a clinic visit for telemedicine. Just because we didn’t get that passed doesn’t mean that all insurance companies won’t step up to the plate and understand that their patients need that as an option for getting their care,” she said. “And it does call attention to the fact that it’s an important part of practicing medicine now, since the pandemic occurred, and will remain an important part.”
PUBLIC HEALTH: Vaping finally regulated, COVID-19 response mixed
By Sean Price
Texas public health won a long-awaited victory by putting vaping products on the same regulatory footing as products made with tobacco.
Senate Bill 248 by Sen. Nathan Johnson (D-Dallas) requires those who sell vaping products to obtain a permit from the state comptroller, just as those who sell tobacco products do. The comptroller’s office can impose fines on those who violate the law.
“This will put a regulatory structure on e-cigarettes in the state of Texas,” said David Lakey, MD, vice chancellor for health affairs and chief medical officer at The University of Texas System. “This is the logical next step so that we know who is selling e-cigarettes and that they’re following the rules of the state.”
Maria Monge, MD, adolescent division director in the department of pediatrics at The University of Texas at Austin Dell Medical School, testified before the House Ways and Means Committee that requiring permits for retailers and penalties for underage sales of tobacco products have successfully decreased adolescent smoking rates.
“As e-cigarettes are both dangerous in their own right and because they are a gateway to other tobacco products, the regulation and enforcement mechanisms for e-cigarettes should be the same as those for tobacco products,” she said. “This bill takes important steps to recognize the serious health risks of vaping and to limit youth access to e-cigarettes.”
Dr. Monge spoke on behalf of TMA as well as the Texas Pediatric Society, the Texas Public Health Coalition, and Texas Tobacco Control Partners – a typical example of how TMA worked with coalitions to achieve legislative success.
SB 248 is definitely a win for public health, but it leaves unfinished an equally important task: taxing vaping products at the same rate as tobacco products, says John Carlo, MD, former medical director of Dallas County Health and Human Services.
Fortunately, this year’s victory on regulation tees up the taxation discussion for the next legislative session, he says. “We seldom come out [of a legislative session] with clean wins.”
That was certainly true in the Texas Legislature’s reaction to the COVID-19 pandemic. Lawmakers passed roughly 20 bills that will change the way the state responds to the next pandemic or public health crisis.
TMA supported many of those bills. For instance, Senate Bill 969 authored by Lois Kolkhorst (R-Brenham), gives the Texas Department of State Health Services (DSHS) more authority to collect health data during a public health disaster and requires the agency to share that information with the public.
Others bills have a more complicated overall impact, says Keller pediatrician Jason Terk, MD, head of the Texas Public Health Coalition.
For instance, Senate Bill 968, also authored by Senator Kolkhorst, is a sweeping bill that, among other things, forbids Texas businesses from barring a customer’s entry or receipt of services based on that customer’s COVID-19 vaccination status. The same bill also helps to set limits on how local health authorities can respond during a declared state of disaster and creates a legislative oversight board to supervise public health disasters. All of these were positions TMA attempted to modify.
“Basically, this is a way for [legislators] to tap the brakes on actions by the governor’s office and local health authorities,” Dr. Terk said.
On the other hand, the bill creates a state stockpile of personal protective equipment (PPE) and establishes the office of a state epidemiologist – measures TMA supports, says Troy Alexander, a TMA legislative affairs director.
TMA’s efforts to improve other pandemic-related bills frequently paid off, he says. For instance, an earlier version of SB 968 required the state epidemiologist to report to the Texas Division of Emergency Management, not DSHS – the state’s public health authority.
Dr. Carlo and others testified before the House State Affairs Committee against making the change.
“Shuffling the oversight of the chief state epidemiologist during constrained times of public health disasters will only create confusion throughout the state as to which entities serve in what roles,” he told lawmakers.
TMA’s work helped ensure that the office remained under DSHS.
The new restrictions placed on public health entities came as an obvious backlash against the measures used to combat COVID-19, Dr. Carlo says.
“We heard quite a bit of opposition to the Centers for Disease Control and Prevention and the National Institutes of Health recommendations [on COVID-19], and a lot of stuff we don’t like to see around anti-science and anti-vaccines that normally don’t have as loud a voice as they did this session,” Dr. Carlo said.
Given this atmosphere, public health champions focused much of their energy on stopping bills that would have hurt public health, Dr. Terk says. TMA-backed efforts were successful in shooting down several bills that would have damaged vaccination and other public health initiatives.
“We were able to get some wins [in public health], but the overall strain of populism over science resulted in a lot of bad bills that needed to be fought,” Dr. Terk said.
One casualty of this year’s session were bills designed to reform ImmTrac2, the state’s immunization registry. TMA-backed House Bill 4272 by Rep. Stephanie Klick (R-Fort Worth) would have, among other things, improved ImmTrac2’s interoperability with electronic health records and simplified the way people give consent on whether to have their records stored in the database. The bill also would have extended the life of disaster-related vaccine records such as those for COVID-19 from five to seven years.
Unfortunately, the legislation got caught up in a political controversy over requiring vaccine passports for COVID-19 immunizations, Mr. Alexander says. Representative Klick passed the original bill through the House with unanimous support, but it died in the Senate on the next to last day of session, he says.
Other TMA-supported public health measures that passed included:
• Preserving $476.9 million in funding for HIV prevention and treatment.
• A $339 million increase in behavioral health funding, including funding for new state hospital construction.
• Senate Bill 1353 by Sen. Borris Miles (D-Houston), which will require DSHS to report immunizations by race, age, and county. DSHS also will be required to recommend ways to decrease inequities in vaccine administration.
• Senate Bill 239 by Sen. Beverly Powell (D-Burleson), which directs DSHS to create a system to provide immunization information and make immunization awareness materials available for local health authorities during a disaster.
• Senate Bill 437 by Cesar Blanco (D-El Paso), which creates an advisory committee on state planning for PPE reserves made up of health care professionals to ensure community and private practice physicians are considered in allocations.
MEDICAL EDUCATION: Lawmakers invest in Texas’ future
By Sean Price
Going into the 2021 legislative session, Texas medical educators were understandably nervous.
The economic fallout from the COVID-19 pandemic had thrown future growth of graduate medical education into doubt.
Texas Comptroller Glenn Hegar projected in July 2020 that the pandemic had created a state deficit of $4.6 billion. In response, Texas Gov. Greg Abbott directed state agencies to adjust their budgets for 2021 to reflect a 5% reduction, with some exemptions, which resulted in a $7 million cut in 2021 to the state’s Graduate Medical Education (GME) Expansion Grant Program
While the program was able to absorb the initial blow without hurting residency programs, the problem was ensuing proposals for the state’s 2022-23 biennial budget called for even deeper cuts.
Fortunately, that fate was averted when in May, the comptroller’s office revised the deficit to a $725 million surplus. In the final 2022-23 budget, at the urging of Senate budgetmakers, the Texas Legislature allocated an additional $49 million for the state’s GME Expansion Grant program, an increase of 27% for a total of $199.1 million, according to Stacey Silverman, assistant commissioner of the Texas Higher Education Coordinating Board (THECB).
More than 400 first-year residency positions have been created through the grant program since 2014, including 135 during the state’s 2020-21 biennial budget period, says Marcia Collins, associate vice president for medical education at the Texas Medical Association. Without a funding boost, there would be no money to refill the newly created first-year positions or to create another round of first-year positions. (See “GME Momentum,” April 2021 Texas Medicine, pages 20-25, www.texmed.org/GMEMomentum.)
That might have forced GME programs statewide to cut funding for up to 170 first-year residency positions statewide by July 2022, says Woodson “Scott” Jones, MD, vice dean of GME and designated institutional official for the UT Health San Antonio Long School of Medicine.
In written testimony for the Senate Finance Committee, then-TMA President Diana Fite, MD, praised lawmakers for their past commitment to “building and expanding the state’s physician workforce pipeline through the generous support of a variety of state programs.” But, she added, “Texas needs an additional 250 first-year GME positions by 2024 to maintain the state’s target ratio of 1.1 to 1 for the number of first-year residency positions per Texas medical school graduate.”
Meeting that ratio is important to keep new physicians in Texas, Dr. Jones says.
“If we keep them in state for both GME and medical school, we have an 80-plus percent likelihood that they’ll stay and practice in the state of Texas,” he said. “And it goes down to about 50% if they leave the state for their GME.”
The improved funding lawmakers ultimately approved should maintain existing residency positions and pay for about 50 new first-year residency slots statewide through the next biennium, Ms. Silverman says.
That’s extremely happy news, says Jonathan MacClements, MD, associate dean of GME at The University of Texas at Austin Dell Medical School.
“The GME expansion [grant program] maintained and increased in size because in the midst of all things COVID, [lawmakers] realized that ensuring that we had a future workforce in the health care professions was clearly [needed],” he said.
Despite growth in expansion grant funding, some physician workforce pathway programs still sustained cuts of up to 5%, says Ms. Collins. They include the Family Practice Residency Program, Statewide Primary Care Preceptorship Program, and Joint Admission Medical Program. Also, the State Physician Education Loan Repayment Program was cut by 3%.
Nevertheless, GME benefited during this session, and Sen. Jane Nelson (R-Flower Mound), chair of the Senate Finance Committee, was a critically important advocate, Dr. Jones says.
“We’re ecstatic with the support in a very tight budget year,” he said.
Physician-legislators like Sen. Donna Campbell, MD (R-New Braunfels), and Sen. Charles Schwertner, MD (R-Georgetown), also were instrumental in boosting the overall GME funding levels.
State lawmakers also allocated $385 million for medical student education, about $45,000 per student, for each year of the 2022-23 budget. They added $49 million to contribute to teaching costs for residents, or about $5,700 per resident, for each year of the biennium. These amounts were largely unchanged from the previous budget, Ms. Collins says.
In a surprise move, lawmakers added $80 million to the state budget at the last minute to help fund the state’s the health science centers. Details about how the $80 million will be spent will be determined in the coming months, Ms. Collins says.
Tex Med. 2021;117(8):20-39
August 2021 Texas Medicine Contents
Texas Medicine Main Page