
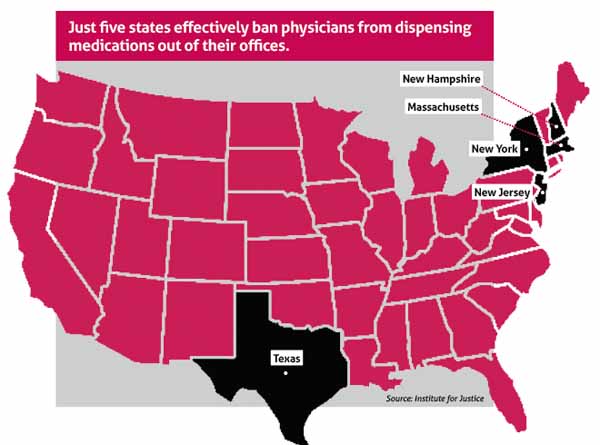
Only a handful of states effectively ban physicians from dispensing medications out of their offices. Texas is one of them.
Medicine has long believed that the state’s general ban on that practice is hurting patients by unnecessarily costing them money and convenience, which, in turn, negatively impacts medication adherence.
Multiple times, the Texas Medical Association has backed legislation to repeal the physician-dispensing ban since the state legislature passed it 40 years ago. None of those efforts have panned out.
But two Texas physicians have taken their case to the courts, arguing that the ban is unconstitutional because it does more to protect pharmacies than it does to protect patients. And TMA is lending its support to that argument.
Austin family physician Michael Garrett, MD, and San Antonio ophthalmologist and eye surgeon Kristin Held, MD, are making that case in a lawsuit against the Texas State Board of Pharmacy (TSBP) and the Texas Medical Board (TMB).
Drs. Garrett and Held are seeking the right to dispense the medications at cost, meaning they would draw no profit from doing so. They argue it’s every bit as safe as pharmacy-dispensing, and physicians across Texas are just as qualified to do so as their rural peers who benefit from exceptions in the law.
Dr. Garrett told Texas Medicine he believes a significant slice of his patient panel would benefit from similar access, “just based on the comments of literally hundreds of my colleagues over the last seven years that do this in other states every day, family physicians. These are routine medications – things like blood pressure medication, diabetes medication, cholesterol medication. They’re routine, bread-and-butter medicines that I prescribe every single day, and I think I could save my patients 40-80% on their costs.”
Irrational and unconstitutional
Drs. Garrett and Held first filed their lawsuit in a Travis County district court in 2019. The trial court threw out the lawsuit, but the physicians appealed their case to the Third Court of Appeals. At press time in late May, TMA was preparing a friend-of-the-court brief to support them.
TMB and TSBP declined comment for this story, citing the pending litigation.
The physicians’ suit partly argues that outlawing physician dispensing violates multiple parts of the Texas Constitution, including an equal-protection section that “forbids the legislature from drawing irrational, oppressive, and protectionist distinctions between similarly situated groups.”
Part of what makes the physician-dispensing ban “irrational,” Drs. Garrett and Held argue in their appeal, lies in the limited authority Texas does give physicians to dispense.
While the ban “has nothing to do with protecting the health or safety of real patients,” the lawsuit claims, “it does serve another purpose: protecting pharmacies from competition.”
Physicians in rural areas working more than 15 miles from the nearest pharmacy can dispense out of their offices at cost. The other exceptions in the law allow any physician to dispense up to a 72-hour supply of non-controlled prescription medication at no additional charge to patients, and physicians can also distribute free samples.
The practical effect of the current law, the lawsuit claims, is that physicians can dispense only at quantities, prices, and locations “that do not threaten the profits of Texas pharmacies. Pharmacies, by contrast, can dispense an unlimited supply of medication, for a profit, in the most populated areas of Texas – all while enjoying at least a 15-mile zone of protection from competition by the nearest doctor.”
Adds the appeal, “As 45 other states have recognized, doctor dispensing is a safe and effective way to increase patients’ access and adherence to their prescribed medications, which is good for patients, doctors, and the broader healthcare system. As licensed doctors, [Drs. Garrett and Held] are just as qualified as their peers across the country to provide this beneficial service.”
Helping to increase patients’ likelihood to adhere to their prescribed course of treatment reduces the potential “for future medical complications and expenses to patients, insurance companies, and the public as a whole,” the physicians’ filing adds.
Dr. Garrett, who’s part of a two-physician direct primary care practice, is confident that he can dispense medications as safely as a pharmacist.
“I certainly think if I’m able to dispense these medications safely for three days of use, [and] if I’m able to know enough about them to prescribe them, and if I can dispense them for free, then I should be able to just recoup my costs. Which is all we’re seeking to do with this lawsuit to be able to provide these medications,” he told Texas Medicine.
Reasonableness is one thing, but what about the argument that the law is unconstitutional under Texas law? Josh Windham, an attorney representing the two physicians for the Arlington, Va.-based Institute for Justice, says those two aspects go hand in hand.
Mr. Windham told Texas Medicine courts have to look at a state law’s “real-world effect” to make sure it’s furthering a legitimate government interest “in a way that’s not oppressive.” There has to be a proper proportion “between the law’s means and its end,” he says, and the Texas physician-dispensing law doesn’t have that.
“The law wasn’t actually designed to further a legitimate government interest,” Mr. Windham said. “It was designed to protect pharmacies from competition, which is not a legitimate use of government power – picking winners and losers in the marketplace.”
In a district court filing responding to the lawsuit, the Texas State Pharmacy Board argued that the laws being challenged do promote safe dispensing.
“While physicians specialize in diagnosis and treatment, pharmacists specialize in drug products and related treatment. After all, pharmacists receive greater education in pharmacology than physicians and thus begin their career with superior pharmacological knowledge on a wider range of drugs than physicians.”
TSBP also claimed the drugs the doctors had identified as ones they “would likely dispense include dangerous drugs that could result in serious adverse health consequences.”
The laws at issue, TSBP claimed, “mitigate against conflicts of interest that may arise when prescribers dispense the drugs they prescribe.” Even if the physicians only seek to recoup costs, “they have a financial interest to dispense medication they purchased and have in stock and to do so before it expires regardless if a different, newer, cheaper, or more effective alternative is available,” the pharmacy board claims. It also argues that the physicians’ argument about equal protection fails because they aren’t “similarly situated” to the rural prescribers who can dispense.
Momentum from Montana
The tide of allowing physician-dispensing across the nation continued its flow last May.
Following a separate Institute for Justice lawsuit in Montana, that state became the 45th to green-light physician dispensing when Gov. Greg Gianforte signed a bill doing so into law. Not only that, but the Montana Pharmacy Association (MPA) publicly admitted “that the organization had previously opposed similar legislation to protect its own business model,” according to a story in U.S. News & World Report.
“Having a group like the MPA say the quiet part out loud, having them say, ‘This has always been about protecting our profits. It’s not been about protecting patients’ – that was all the Montana legislature needed to do the right thing,” Mr. Windham told Texas Medicine. Meanwhile, following passage of Texas’ physician-dispensing ban in 1981, he says, “the Texas Pharmacy Association (TPA) has stepped in ever since, every time a reform has been proposed, to effectively have it shot down in the legislature.”
TPA did not return a phone call from Texas Medicine seeking comment.
TMA backed an ultimately unsuccessful effort to lift Texas’ ban during the 2019 legislative session, which included House Bill 1622 by Rep. Tom Oliverson, MD (R-Cypress). After that session, TPA said the proposed physician-dispensing measures “would have threatened patient health and safety by not requiring the same high standards as pharmacist-dispensing or the same Texas State Board of Pharmacy oversight to protect patients.”
Tex Med. 2021;117(7):45-47
July 2021 Texas Medicine Contents
Texas Medicine Main Page