
If you’ve been in practice long enough, chances are you remember an era when some of today’s for-granted technology was a curio.
Email use in health care was a novelty that required new guidelines and protocols. Later down the line, text messaging was considered similarly newfangled, offbeat, and impersonal.
Telehealth, to some degree, is in that same place right now. But after the COVID-19 pandemic and a desperate, largely telemedicine-or-nothing era of health care, it’s careening into more widespread, everyday use and acceptance, much like emails and texting did over the past two to three decades.
The Telehealth Initiative – a program launched in January 2020 by The Physicians Foundation, American Medical Association, Texas Medical Association, Florida Medical Association, and Massachusetts Medical Society – didn’t anticipate the pandemic. But it did anticipate telemedicine’s potential wealth of applications for care. And when the pandemic hit – two months into the initiative’s yearlong quest to educate physicians and practices on telehealth and promote its use – telemedicine became more of an on-the-job training proposition than any participant had imagined.
(Although telemedicine and telehealth are often used interchangeably, telehealth generally refers to providing care using remote technology, while telemedicine is specifically the practice of medicine using that technology.)
Ultimately, Texas physicians who participated in the Telehealth Initiative say that into-the-fire necessity was a positive.
“Without the pandemic, we would be not progressing on telehealth and not understanding telehealth,” says Shenandoah family physician Bharat Latthe, MD, one of the physicians who took part in the initiative. “The pandemic actually helped us to go forward on telehealth and understand the benefit to patients and doctors. Everybody benefited from the pandemic [in the sense] of jumpstarting telehealth.”
With TMA providing a helping hand, the Telehealth Initiative taught physicians a lot and learned from them in return. Now, TMA and others in organized medicine are looking to maximize telehealth’s potential, with other remote technologies holding promising possibilities.
Realizing the benefits
As part of the 12-month trial program, the initiative lent its assistance to 24 practices and 168 clinicians. According to an issue brief (tma.tips/TIbrief), the program’s activities included six webinars, two extended virtual boot camps, and two methods to measure success and gather feedback, and created more than 100 resources.
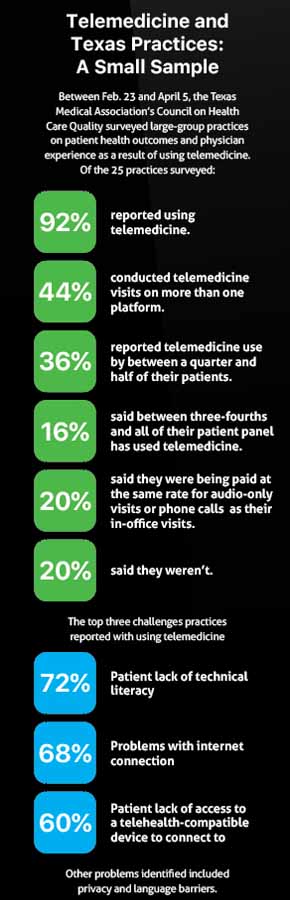
A survey conducted in the midst of the program showed most participating practices were currently using telehealth, with 75% saying COVID-19 affected their decision to implement it sooner than anticipated.
“Topics covered throughout the program included telehealth vendor evaluation and selection, designing telehealth workflows, engaging patients, and addressing equity. As an outcome of the program, all participating practices recruited by the state societies reported adoption of telehealth despite the accelerated timeline forced by the COVID-19 public health emergency,” the issue brief said.
Resources that physicians used as part of the initiative are now available for any physicians looking to upgrade their telehealth capabilities and literacy. (See “Telehealth Resources for All,” page 25.)
The Telehealth Initiative conducted one-on-one interviews with physician participants in November 2020. Before the program started, according to those interviews, participants in general didn’t have telehealth established.
“While some did provide telehealth [beforehand], it was rarely used by patients, and the platforms were often cumbersome,” the issue brief said. “After the Telehealth Initiative, most were primarily using live audio-visual telehealth appointments to see patients, and some physicians reported to default to alternative platforms or audio-only phone visits if they or their patient was having technical issues accessing the video platform. Practices’ percentage of telehealth visits varied over the first months of the pandemic and the majority are now conducting a mix of in-person and telehealth.”
Dr. Latthe was one of those participants who had no experience with telemedicine prior to the initiative. So was Round Rock family physician Tina Philip, DO, who signed up for it knowing she was about to open her solo practice in March 2020 – as it turned out, the month when the pandemic upended the world.
“Going into [the initiative], my mindset was, ‘I want to add this as an extra service.’ But because of the pandemic, it became, ‘This is how I’m going to have to practice medicine if I want to see patients at all,’” Dr. Philip told Texas Medicine. “So it was definitely a big shift in terms of how I saw telemedicine initially as an add-on versus, ‘This is solely how I am practicing for a couple of months.’
“It would have been really daunting, having to start the practice and start doing telemedicine without any help at all. So it was nice to have that initiative in the background as a resource.”
With just herself and two office workers, Dr. Philip had the help she needed from TMA staff supporting the program. She didn’t have to search on her own for the procedural nuts and bolts of setting up telemedicine, like how to obtain patient consent to do a televisit.
“TMA staff were able to give us a little bit of one-on-one guidance, too, specifically, ‘My practice is having this issue. I don’t know what to do.’ They did check in with us periodically throughout the whole process to say, ‘How are things going? What issues are you having? What can we help you do?’” Dr. Philip said.
“TMA was really great about [putting] together paperwork, consent forms and things like that for patients regarding telemedicine, and helping us with billing, and what codes should we be billing, and how to get paid for [it].”
Physicians using telehealth for the first time saw just how much it could do, both with respect to convenience and keeping patients safe during the pandemic.
For Dr. Latthe, the Shenandoah family physician, the average age of his patients is 75 years old.
“So you can imagine a 75-year-old lady trying to reach my office in the busy traffic, [she] can’t see, and tries to find a parking spot, come inside, sit here in the waiting room for a long time. While she’s waiting in the waiting room, she’s going to be worried about who’s sitting next to her and coughing, and is she going to get COVID from that patient. Whereas she can make a call, I can do a televisit with her and take care of her problems,” he said.
Now that he’s established the technology, “out of 10 or 15 or 20 televisits, I may have to call one patient to come to my office. The rest of them, I can take care of them with televisits.”
 Denton OB-Gyn Joseph Valenti, MD, said the initiative was “the right thing at the right time.” It helped his practice connect with its wide service area. He is one of two TMA members serving on The Physicians Foundation’s Board of Directors.
Denton OB-Gyn Joseph Valenti, MD, said the initiative was “the right thing at the right time.” It helped his practice connect with its wide service area. He is one of two TMA members serving on The Physicians Foundation’s Board of Directors.
“I’m in very, very north Texas. So, it actually expanded the catchment area for the practice because we were able to see people from far away. And especially for pre- and post-operative visits, I had patients coming from an hour and a half, two hours away. So instead of coming in for a 20-minute visit, we did it over the phone and saved them a ton of time. Obviously, the mitigation of the infection risk was huge,” Dr. Valenti said.
“We were able to see people who also were sick over the phone, or through telehealth, that otherwise would not be allowed in the office in any case, or wouldn’t want to come in in any case. It also allows you to avoid some [emergency department] visits, if you can look at some stuff over the phone or through video and be able to diagnose things that would keep people out of the emergency room.”
With little time to prepare due to the pandemic, the virtual boot camps and other learning sessions, Dr. Valenti added, “would have been more important had we not had COVID. But because COVID forced our hand, everyone was kind of immediately forced into [telehealth]. They didn’t have time to really spend a lot of time getting ready – ‘Gotta go do it.’ There were a lot of places that didn’t have any other business. Everyone was taking their [Paycheck Protection Program and Economic Injury Disaster] loans just to try to stay afloat.”
Patients’ acceptance of telemedicine was ultimately one of the biggest surprises for Dr. Valenti: “They were very satisfied, and I didn’t think they would be.”
Less joy, more stress?
During feedback sessions the Telehealth Initiative conducted with participants, interviewees reported their perceptions of telemedicine were generally positive, but they identified negative impacts, too, according to the issue brief.
On the positive side, physicians’ feedback represented much of what Texas participants relayed to Texas Medicine. Physicians polled by the Telehealth Initiative said telehealth provided:
- Convenience;
- Easier access to care for patients with schedule limitations or transportation challenges; and
- The ability to deliver care that many patients would otherwise have delayed or neglected during the pandemic.
On the other hand, one physician who participated in the initiative said virtual patient encounters are less joyful than in-person visits, and several doctors said the stress of adding televisits to their office schedule contributed to burnout.
“Some practices had a difficult time adjusting to the changes that came with the pandemic and incorporating telehealth, but with that challenge came innovation and adaptations of practice workflows, using new care protocols and team-based care,” the issue brief said.
In an interview with Texas Medicine, Virginia pediatrician Russell Libby, MD, a member of The Physician Foundation’s board, confirmed that some participants had a harder time than others.
“There were some who found it difficult, that never really did develop an adequate platform,” he said. “They didn’t necessarily feel confident or comfortable with the kind of work they were doing, evaluating patients, and didn’t necessarily connect well with patients doing a virtual connection.”
Dr. Valenti also saw firsthand another unfit piece of the puzzle: A lack of universal high-quality internet access.
“I was very surprised how many patients had either no reception or poor reception. That was a bit of a challenge,” he said. “I was amazed how many telehealth visits I wanted to do over video, but because of technological challenges, we had to do them over the phone. A lot of patients don’t have the connectivity or the technology to do what we needed to do, depending on where you are.”
At press time, TMA-supported legislation to expand Texas’ broadband capability had passed the Texas Legislature and was awaiting Gov. Greg Abbott's signature. Federal legislation that would make telemedicine easier for both physicians and patients also was on TMA’s radar.
Where to now?
Even after its successful, accelerated coming of age, more is on the horizon for both telemedicine and associated technology. At the same time, a wealth of work remains to realize the full potential of telemedicine and those other technologies.
AMA is using the Telehealth Initiative as a framework for its Telehealth Immersion Program, AMA’s newest guide to helping physicians optimize and sustain telehealth using similar methods. (See “Immerse Yourself in Telehealth,” page 24.)
Meanwhile, Dr. Libby said in May that the Telehealth Initiative was working on building a “second cohort” of practices to participate in surveys and quality improvement projects involving telehealth.
He says one issue going forward is developing “resources that are continuously being evaluated and updated,” which requires both investment and awareness that telehealth will continue to evolve. Remote exam tools, for example, offer the opportunity for patients to hold a portable stethoscope against their chest, and have their physician use a Bluetooth device to evaluate their breathing.
“You have a load of remote monitoring devices that can continuously report to an [artificial intelligence] kind of platform that helps to reduce and select out useful information for the physician to review and to respond to a particular patient in a more effective and comprehensive manner,” Dr. Libby said. “It’s like this year has just slapped the baby on the bottom, and the baby’s screaming. Yes, we’ve got to learn how to use this and make it work to the benefit of patients and the profession.”
However, skepticism about some of those remote technologies remains in the physician community. Dr. Latthe, for example, sees something like remote electrocardiogram (ECG) monitoring as “more of a gimmick,” because if a patient needs an ECG, it means the patient is extremely sick.
“My opinion is sick patients with complex medical problems, I think if they need such extensive monitoring, that probably [it’s better to see them] in the clinic,” Dr. Latthe said. “But newer gadgets will be available. That might help, and we might be able to do that. But at this time, I just don’t feel comfortable doing telehealth on very sick patients.”
Dr. Libby says combating insurance payer resistance to telehealth’s advancement will be a major part of what comes next. Central to that piece is collecting more data “to show that what we’re doing through telemedicine actually improves outcomes, improves care, improves both professional and patient satisfaction, and ultimately saves the health care system a lot of money.”
So, the biggest part of the Telehealth Initiative’s second act, he said, “is to teach docs how to do that kind of research in their day-to-day operation and to look at their processes and to be able to refine them and improve them based upon the data that they can accumulate and how they can have that analyzed. And help them find ways to demonstrate the value, the cost savings, and improve on that as they operate.”
Tex Med. 2021;117(7):20-25
July 2021 Texas Medicine Contents
Texas Medicine Main Page