
As the Centers for Medicare & Medicaid Services continues to churn out glowing data annually on its Quality Payment Program (QPP), a full picture of the program’s impact eludes the agency’s reporting. According to the Texas Medical Association’s analysis of state-level data in the 2018 QPP Experience Report, it’s clear that small practices continue to feel most of the program’s punitive pressures.
The Texas data reflects participation in the Merit-Based Incentive Payment System (MIPS), one of two tracks in which physicians can participate in the QPP; the other track is an advanced alternative payment model (APM).
Although CMS data show that the vast majority of MIPS participants, both in Texas and nationally, continue to meet the program’s scoring thresholds for earning payment incentives, small practices are getting “disproportionately” penalized, says San Antonio rheumatologist Chelsea Clinton, MD, chair of TMA’s Council on Health Care Quality. And the Texas statistics contain no details on the state’s advanced APM participation, leaving medicine partially in the dark in its push to advocate for QPP improvements.
“That’s a large hole in the program,” Dr. Clinton told Texas Medicine. “By us not having information, it makes it so that we [aren’t] able to make … recommendations. We don’t have the data that we need to help our cause.”
CMS acknowledged an interview request from Texas Medicine but did not make anyone available and did not submit answers to written questions by press time.
Small practices pay the price
CMS’ initial 2019 QPP Experience Report portrayed astounding success for the program’s inaugural year in 2017. But a TMA analysis at the time found the report contained a lack of detail and transparency, and questionable data. (See “A False Impression,” June 2019 Texas Medicine, pages 32-37, www.texmed.org/falseimpression.)
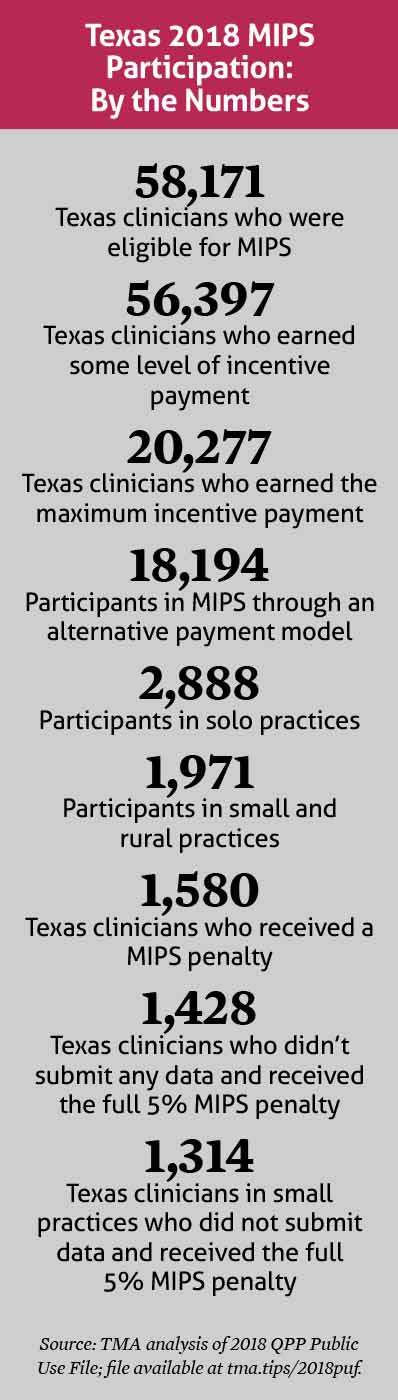
In TMA’s view, the 2018 Texas data are more of the same. (See “Texas 2018 MIPS Participation: By the Numbers,” right.)
Based on the performance numbers CMS released, it would seem Texas MIPS participants – physicians as well as other clinicians – are doing well. TMA’s high-level analysis of the CMS data indicates that 97% of MIPS-eligible clinicians received some level of incentive payment, and roughly a third earned the maximum incentive payment of 1.68% of their practice’s Medicare billings.
But TMA staff believe that given the miniscule “positive payment adjustments,” or incentive payments, available in QPP, most practices are really just avoiding a penalty. And other data illustrate who’s taking the hits.
Of those Texas physicians earning the maximum payment penalty of 5%, which came due in 2020, 83% were small practices, which CMS defines as practices with 15 or fewer clinicians.
The results continue to show one of the overarching concerns with QPP – that because it’s a budget-neutral program, its penalized “losers” foot the bill for the “winners” who earn incentive payments, TMA experts say.
TMA’s research also concludes that CMS’ incomplete, selective reporting on the program continues.
For example, although the state-level data noted that 18,194 Texas participants did so through a MIPS APM, it contained no information on which models participants used, or how many Texas clinicians participated through an advanced APM. That data is necessary to chart the state’s transition from traditional fee-for-service into value-based care, TMA experts say.
Although CMS says QPP is risk-adjusted to account for practices’ unique circumstances, TMA’s research points out the program contains no adjustments for social determinants of health, which can have an outsized impact on a practice’s outcomes, especially if a practice cares for a high number of socially disadvantaged patients.
What’s more, the maximum penalty for failing to hit the annual MIPS target keeps increasing. The 2019 performance-year maximum penalty was 7%, which will be assessed this year. For 2020, the maximum penalty was 9%, which will affect penalized practices in 2022.
“Getting these penalties ... can be devastating to a practice, especially when probably a good percentage of their practice is Medicare,” said Austin otolaryngologist Jeffrey Kahn, MD, immediate past chair of the Council on Health Care Quality. “It may really be very, very tough for rural and underserved practices, especially in medical and underserved areas, to keep up if they keep getting dinged 7-9%.”
The ultimate goal
The bottom lines of QPP, Dr. Kahn notes, are supposed to be improving quality and reducing costs. And the question of whether it’s achieving those objectives also goes unanswered in the CMS data.
“We know people are able to check boxes and satisfy criteria, and we’re doing that same thing in our practice through our EHR, but it’s still kind of a game,” Dr. Kahn said. “[Physicians say], ‘Well, this is either stuff I’m already doing, and now I have to spend time documenting in greater detail that I’m doing it, or … maybe I’m going to just find a way to game the system by picking those metrics where I can do the least amount of work possible.’
“It all comes down to this game that I think a lot of practices are playing, and it’s unclear if that truly translates into better quality care. We also don’t even know if this is reducing costs, because that’s what this was also supposed to do.”
TMA has and will continue to advocate to CMS for improvements in QPP to make the program fairer and less burdensome and onerous, including elimination of the requirement that the program be budget-neutral. TMA believes the detrimental impact that requirement has on small practices is already showing up in the numbers, and the program’s penalties continue to rise.
“There’s a lot of good that small practices have to offer, and I don’t really like the trend that we’re experiencing of promoting larger and larger practices,” Dr. Clinton said. “Because larger practices can run into the same issue in regards to customer service and other problems that hospitals have and very, very large companies have. A variety is better.”
Tex Med. 2020;117(1):32-33
January 2021
Texas Medicine ContentsTexas Medicine Main Page