Public Health Priorities
Expand Health Care Coverage
Telemedicine: Proof for Parity
STAYING THE COURSE
By Joey Berlin
The way the Texas Legislature conducts business will change. The Texas Medical Association’s commitment to improving health care won’t.
But to make that happen over the next four months, TMA may need your help – your engagement – more than ever.
At this writing, the legislative format for the 2021 session was still an unknown: How much of the activity would take place in person under the Pink Dome? How much would be virtual? Would the COVID-19 pandemic mean fewer bills could earn consideration and advancement through the legislative calendars?
“It is going to be like no other session because of the pandemic,” said Austin oncologist Debra Patt, MD, chair of TMA’s Council on Legislation. “And while we don’t know exactly what the 87th session will look like, having TMA members communicate with their elected officials in their district by phone, by Zoom, is going to be really important. Because medicine will have a decreased physical presence in the Capitol because of increased restrictions, due to the pandemic.”
Sen. Dawn Buckingham, MD (R-Lakeway), one of five physician members in the 2021 legislature added: “We’re trying to figure out how to safely, from a health perspective, be sure that we maintain the public’s access to government while also not endangering our staff. There’ll be fewer bills heard. I think the committees will be more spread out.”
But for TMA, the general goal is the same: protecting and advancing the practice of medicine in Texas.
Top-line items: The budget and more
TMA Vice President for Advocacy Dan Finch says medicine’s aims will begin with the only thing the state constitution requires the legislature to do when it convenes: Pass a two-year budget.
Although there were many unknowns at press time, what was known is that the pandemic has taken a profound toll on the state’s fiscal outlook. Comptroller Glenn Hegar projected in July that the economic consequences were severe: Instead of a surplus of about $3 billion, the state will face a deficit of about $4.6 billion. As a result, state leadership asked a number of state agencies, including the Texas Department of State Health Services, to submit budgetary plans that would include a 5% cut.
From that less-than-ideal starting point, medicine will be trying to secure its share of funding as legislators also attempt to mete out funds for public education.
“The legislature put about $11 billion last session of new monies into public education support. They’ll be looking to maintain that support,” Mr. Finch said. “Remember, the two biggest areas the state funds are health care and education.”
Those two areas have been a main focus for the state during the pandemic. Lawmakers also will be preoccupied with redrawing the state’s political maps, which Mr. Finch says is likely to be addressed during special sessions this summer.
Against that backdrop, medicine’s top-priority budgetary goals include:
- Ensuring strong eligibility and enrollment in Medicaid, and improving access in the program, including some form of meaningful coverage expansion, aimed largely at the working poor in Texas.
- Maintaining and, if possible, increasing current physician payment rates in Medicaid, which haven’t seen a meaningful increase in more than two decades.
- Increasing continuous coverage of children on Medicaid to 12 months, instead of the current six months, and provide 12 months of comprehensive coverage for women who lose Medicaid 60 days postpartum.
- Building on last session’s gains in graduate medical education, in which TMA secured a funding increase of more than $60 million, and maintaining the ratio of 1.1 residency slots for every medical school graduate as class sizes continue to grow.
- Restoring funding for the Family Medicine Residency Program and the Physician Loan Repayment Program, both of which the legislature reduced funding for in recent sessions.
- Making gains in funding for essential public health services, including funding to make the exchange of data between county health departments and the state more operable, continuing to promote needed vaccines, and boosting mental health services.
Along with the financial difficulties the pandemic has wrought, Dr. Patt notes that legislators will be reluctant to fully tap into the state’s reserves, the Economic Stabilization Fund, known informally as the “rainy day fund.” But, she says, there’s never been a time when the state’s medical infrastructure needed continued funding more.
“Access to care is a big priority for TMA not just because such a high percentage of adult Texans are without insurance, but also because, when such a high percentage of adult Texans are without insurance, it really becomes not only a tragedy, but also a medical liability issue,” Dr. Patt said. For instance, hospitalized patients who can’t comply with discharge instructions because of lack of insurance can end up in the hospital again.
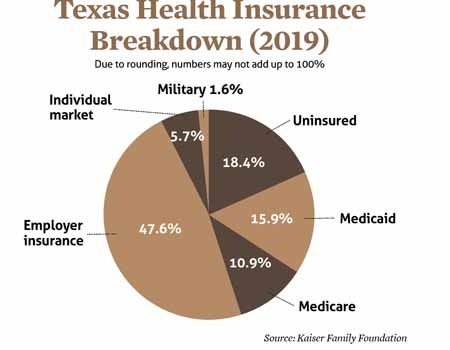
The U.S. Census Bureau’s latest report, analyzing 2019 health coverage, pegged Texas’ overall uninsured rate at 18.4% that year. Because the uninsured rate rises as the unemployment rate increases, that number has grown because of the pandemic, but estimates vary as to how much. (See “Expand Health Care Coverage,” page 24.)
But along with its disruptive and demoralizing negatives, the pandemic has created an opportunity for medicine to bend lawmakers’ ear on some of its longstanding goals.
For instance, COVID-19 has spotlighted the state’s access-to-care problems, and it necessitated a headlong, successful dive into telemedicine for both physicians and patients. As it has in previous sessions, the house of medicine aims to perpetuate telemedicine’s success during 2020 with legislation mandating permanent payment parity, meaning insurers must pay the same for telemedicine that they do for the same covered services provided in-person.
TMA lobbyist Michelle Romero believes that the emotional toll of COVID-19 also will help TMA make the case for greater funding to address substance use disorder and suicide prevention.
Texas is “already making strong investments in behavioral health, mental health,” she said. “But I think the pandemic is going to really put a big focus on continuing to ensure that those dollars are there, and that Texans are getting access.”
TMA also will look to build on previous legislative gains in restricting the prior authorization hassles that health plans levy upon physicians, and the delays in care they cause.
Stalwarts at the Capitol, on the phone
Following the November 2020 elections, the makeup of the legislature looks much like it did during the 2019 session. The party breakdown of the House of Representatives remained the same: 83 Republicans, 67 Democrats. In the state senate, Democrats picked up a seat, slightly whittling the Republican majority to 18-13.
But much more importantly for TMA, the legislature will once again contain many friends of medicine in both parties. Candidates endorsed by TEXPAC, TMA’s nonpartisan political arm, won nearly all their races in the November general election.
The 2021 legislature will include five physicians upon whom medicine will rely to communicate and advance physicians’ interests. Senator Buckingham, the only physician in the Senate who was on the ballot in November, won reelection. She’ll be joined in the upper chamber by Sen. Donna Campbell, MD (R-New Braunfels) and Sen. Charles Schwertner, MD (R-Georgetown).
On the House side, Rep. Greg Bonnen, MD (R-Friendswood) and Rep. Tom Oliverson, MD (R-Cypress) both easily won reelection in November.
The replacement of House Speaker Dennis Bonnen also could impact medicine’s agenda.
But a handful of members can’t push that agenda through on their own. TMA relies on its white-coated soldiers who bend legislators’ ears during the monthly First Tuesdays at the Capitol. With that event becoming a virtual venture this year, and other white-coat activity at the Capitol almost certainly curbed to a minimum, Dr. Patt urges the house of medicine to follow up its gains in telemedicine with some dogged tele-lobbying.
“Probably the most the important thing is that you pick up the phone and call your elected official,” she said. “Make sure that they are in your cell phone. Make sure they know what issues impact you.”
By Sean Price
Not surprisingly, the biggest public
health crisis in decades will dominate TMA’s public health agenda for the 2021
Texas Legislature.
Job No. 1: rolling back the 5% budget cuts – amounting
to $32.9 million – that the Texas Department of State Health Services (DSHS)
has been asked to make in response to the state’s pandemic-related
financial troubles, says Texas Public Health Coalition Chair
Jason V. Terk, MD.
“Cutting nearly $33 million from the state’s top public
health agency simply should not be on the table during a pandemic,” Dr. Terk
said. “Our state needs dependable investment in preventing and eliminating
disease threats at all times. Furthermore, funding pandemic response efforts
should not come at the expense of cuts to DSHS’ other important areas of work,
such as tobacco control, chronic disease prevention, immunizations, and
maternal and child health.”
The COVID-19 pandemic coupled with sharp drops in
petroleum prices have slowed the state’s economy and caused drastic shortfalls
in the state budget. Texas Comptroller Glenn Hegar has projected a $4.6 billion
shortfall, and Texas Gov. Greg Abbott asked state agencies to make the 5%
budget cuts. (See “Staying the Course,” page 18.)
For public health, the cuts would mean certain activities
– such as tobacco enforcement and support for addressing child maltreatment in
health care settings – would be eliminated completely, according to DSHS. Other
programs – such as infectious disease surveillance, HIV reduction, and meat
safety – would face partial cuts, the agency says.
DSHS was exempt from similar 5% cuts faced by most other
state agencies in fiscal years 2020 and 2021. Given the pandemic’s impact on
state health, public health officials had hoped for a similar exemption in the
2022-23 biennium, says John Carlo, MD, the former medical
director for Dallas County Health and Human Services and past chair of the
Texas Public Health Coalition.
The agency already has too few staff to adequately combat
the pandemic and provide other necessary services, he says.
“DSHS is not flush with cash to begin with,” Dr. Carlo
said. “This is really, really bad. It’s a huge number.”
Other state agencies that deliver public health services
are looking at 5% cuts as well, including the Texas Health and Human Services
Commission and the Texas Department of Family and Protective Services.
Long-term deficiencies in public health funding have had
a direct impact on the Texas response to COVID-19, including the inability to
hire the necessary staff for epidemiologic investigations and the inability to
track disease data rapidly because of antiquated information systems, says Umair
A. Shah, MD, former executive director and local health authority for Harris
County Public Health.
“We would be so far along the curve if we invested in
public health systems in advance of crises and were not trying to play catch-up
in the middle of these crises,” he said.
Promoting vaccines
People everywhere will be focused on COVID-19 vaccines as a way to
curtail the pandemic during this legislative session, and that should give
physicians an opening to reinforce the importance of all vaccines, says David
Lakey, MD, vice chancellor for health affairs and chief medical officer for The
University of Texas System.
“There will be a lot of conversations about COVID and
vaccinations and funding the public health infrastructure [for vaccines],” he
said. “And that may provide an opportunity to move some of the essential public
health systems forward.”
This emphasis on vaccines dovetails with a new TMA
vaccine education program, “Vaccines Defend What Matters,” recently launched to
address the dramatic drop in vaccinations during the spring of 2020 as the
pandemic increased in severity (www.texmed.org/DefendWhatMatters). Between early March and early June, the pandemic forced most
medical practices to postpone well checks and vaccines. According to DSHS, the number
of vaccine doses administered through the Texas Vaccines for Children (TVFC)
program during that period and beyond was significantly down compared with
2019. (See “COVID-19 Drives Down Overall Vaccination Rates,” below.)
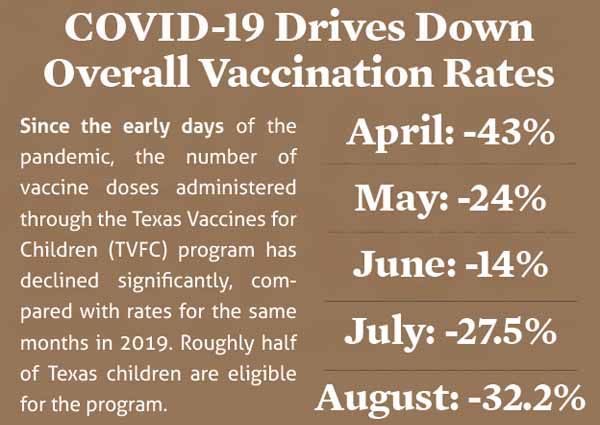
Although initial declines rebounded somewhat in May (24%
lower) and June (14% lower) compared with the same months in 2019, the number
of vaccine doses administered remained well below 2019 levels as of September
2020, according to TVFC data. Roughly half of Texas children are eligible for
the program.
The immunization delays caused by COVID-19 could spark or
worsen outbreaks of vaccine-preventable diseases like flu or measles, says Dr.
Terk, a pediatrician.
The focus on COVID-19 vaccines also may provide
physicians with an opening to limit or improve monitoring for vaccine
exemptions, says Karen Batory, TMA vice president for population health and
medical education.
Even before the pandemic, a growing number of Texas
parents had sought these exemptions for their children. Increasing numbers of
unimmunized students can make a school or neighborhood more susceptible to
disease outbreak. (See “Talk to Patients About: What’s Wrong with Vaccine
Exemptions?” Texas Medicine, May 2020, page 47,
www.texmed.org/VaccineExemptions).
Mental health and more
All of TMA’s public health priorities will have to take into
consideration the state’s tight financial situation, Dr. Terk says.
“This is not the session where we’re going to be able to
have dreamy-eyed projects that we can spend a lot of money on,” he said.
But because of the problems highlighted by COVID-19,
physicians could push the state to prepare for future public health emergencies
by modernizing data systems; training and retaining a skilled disease
surveillance workforce; and stockpiling personal protective equipment,
medicines, and other supplies, Dr. Terk says.
“That is the best way for us to be thinking ahead so that
we not only have plans but material that we can use when, not if, these things
happen,” he said.
TMA can also expect to make headway in mental health, Dr.
Lakey says.
“There’s strong bipartisan support to improve mental
health services,” he said. “The state has moved forward significantly [in
mental health] over the last 15 years, and I don’t think they will want to stop
that momentum.”
Thanks in part to TMA advocacy, the last two legislative
sessions produced big gains in behavioral health care. In 2019, for instance,
lawmakers approved Senate Bill 11, which established the Texas Child Psychiatry
Access Network, giving pediatricians and other primary care physicians access
to a greater range of psychiatrists and other licensed behavioral health
professionals. (See “Use It or Lose It,” December 2020 Texas Medicine, pages
34-37, www.texmed.org/UseCPAN.)
Perhaps the biggest advances in mental health and
substance abuse treatment this year have come in telemedicine as a direct
result of the pandemic, Dr. Lakey says. Physicians can ensure that those
advances remain in place by pushing to make permanent emergency rules that enabled
the widespread use of telemedicine during the pandemic, he says. (See
“Telemedicine: Proof for Parity,” page 26.)
Also, in the last legislative session, lawmakers only
partially funded the Austin State Hospital and San Antonio State Hospital, both
of which provide important psychiatric services, Dr. Lakey says.
“We need to finish the job of funding those two
facilities in this legislative session,” he said. EXPAND HEALTH CARE COVERAGE
By Sean Price
Before the COVID-19 pandemic hit Texas in early 2020, the state had both the highest percentage of residents without health insurance – 18.4% – and the highest number of uninsured – about 5 million, according to an October 2020 report by Texas Comptroller Glenn Hegar.
“And those numbers have risen in 2020 as the COVID-19 pandemic continues, causing economic turmoil and massive job losses,” the report stated.
The latest count by Kaiser Family Foundation puts Texas’ uninsured rate at 20.9% in 2020.
The Texas Medical Association has pushed for state lawmakers to resolve its long-standing problems caused by this lack of health insurance. That starts with Medicaid coverage. Texas is one of only 12 states that have not expanded Medicaid.
“Texas can no longer ignore the profound economic, social, and human impact of having more than 5 million uninsured residents,” TMA President Diana L. Fite, MD, wrote in a Sept. 8, 2020, letter co-signed by the 16 other medical societies to the Texas House Committee on Insurance.
The 2021 legislative session might be Texas’ last chance to expand Medicaid on its own terms and create a truly “Texas plan,” says Austin pediatric cardiologist Hanoch Patt, MD, a member of TMA’s Select Committee on Medicaid, CHIP, and the Uninsured.
The current 1115 Medicaid Transformation Waiver that Texas participates in – which allows the state to expand Medicaid managed care while preserving safety net hospital funding and testing new ways to reform care delivery for Medicaid and uninsured patients – will expire in 2022. It is unlikely that the Biden administration will renew it without getting Texas to agree to Medicaid expansion, Dr. Patt says.
“There’s [been] skepticism both under the Obama administration and the Trump administration – and presumably [there will be under] the next presidential administration as well – about continuing an inefficient mechanism to fund health care for uninsured Texans when a much more straightforward system is available by expanding Medicaid,” he said.
TMA and a diverse array of organizations representing hospitals, faith communities, and consumer advocates continue to urge lawmakers to support meaningful expansion of coverage using federal dollars, says Dan Finch, TMA’s vice president of advocacy.
As in past sessions, Democratic lawmakers already have filed several bills seeking to expand coverage, including Medicaid expansion under the Affordable Care Act (ACA), as of mid-November. Given the economic fallout related to the pandemic, there are glimmers of bipartisan support going into the 2021 legislative session.
“With a very tight budget environment, coverage expansion and its projected positive economic benefits, it might be the time to court Republican support, particularly among those who have rural hospitals in their districts teetering on the financial edge,” Mr. Finch added. “States that expanded Medicaid have had far fewer rural hospital closures.”
Rep. Lyle Larson, R-San Antonio, recently suggested in an October tweet that the state should “seriously consider accessing federal Medicaid funding” this legislative session. “This is money we’re sending to the federal government and not getting back.”
The comptroller’s report acknowledges that states “that chose to expand Medicaid eligibility experience[d] the largest decreases in their uninsured rates,” but goes on to say, “per-person costs for Medicaid expansion have exceeded original estimates by 76%, leading to cost overruns of 157%.”
“When considering policies to address the state’s high uninsured rate, a variety of strategies should be considered,” the report concludes.
Multipronged approach
TMA’s letter called on lawmakers to support a multipronged approach by seeking federal waivers to implement innovative strategies to improve health care coverage under the 1115 waiver and under the ACA.
Texas could expand the 1115 waiver to extend health care coverage to low-income adults 64 and younger in the Medicaid “gap” – the 1.5 million uninsured Texans who are not poor enough to qualify for Medicaid but who still live in poverty, the TMA letter to Texas lawmakers says.
Two recent studies by the Episcopal Health Foundation (EHF) show that expanding Medicaid would not only save Texas money, it could add to the state’s coffers at a time when money is short (www.texmed.org/2020MedicaidStudies).
One of the reports found that a “fully operational, 90% federally financed” Medicaid expansion program – as originally envisioned under the ACA – would save the state more than $50 million per year, or nearly $110 million over a biennial budget.
Expanding the 1115 waiver would allow lawmakers to tailor the program to their liking, says Ken Janda, a Houston-based health care consultant and adjunct professor at Rice University’s Jones Business School. For instance, Georgia’s program includes work-training requirements, and Indiana’s provides extra money for dental and vision to people who can show healthy behaviors, he says.
“We can come up with some creative ideas to utilize the federal dollars to do a Texas solution,” he said. “Other conservative states have figured out ways to use those federal dollars that are available.”
Texas lawmakers also could improve physician participation in Medicaid by paying physicians more competitive Medicare rates for Medicaid services, Mr. Janda says.
“It’s likely that if the state increased [payment] rates for providers that would result in more physicians being willing to see those patients, and care being provided at the right place and the right time, instead of the care being provided in more expensive ways in emergency rooms and hospitals,” Dr. Patt said. “If the state used money more efficiently and increased physician rates it would result in overall less cost [to the state] and better outcomes, with earlier diagnosis and better patient management.”
Covering the other 3.5 million
While about 1.5 million uninsured Texans could be covered by potential Medicaid expansion, the other 3.5 million need better options as well, the TMA letter says.
So far, 14 states have received “1332 waivers” under the ACA that allow them to create state-administered reinsurance programs funded jointly with federal and state dollars, according to the State Health Access Data Assistance Center. These waivers allow states to use the money to reduce health insurance premiums for individuals purchasing coverage via the marketplace but who are ineligible for subsidies.
In the first year of operation, state-run reinsurance programs authorized by 1332 waivers reduced individual market premiums by an average of 19.9%, according to Avalere Health, a Washington, D.C., health care consulting firm.
TMA and the other Texas medical organizations “support pursuit of such a reinsurance-focused 1332 waiver not only because of its potential to help lower the costs of marketplace premiums but also because this type of 1332 waiver is the most likely to be quickly approved by the Centers for Medicare & Medicaid Services,” the TMA letter to Texas lawmakers said.
Like Medicaid expansion, this coverage expansion also would bring in enough federal dollars to save the state money, Mr. Janda says.
However, lawmakers’ deliberations about expanding health care coverage could be overshadowed by California v. Texas, a case heard before the U.S. Supreme Court on Nov. 10, 2020. Texas, 17 other states, and two individuals argued that changes made to the ACA by Congress in 2017 rendered unconstitutional the law’s requirement for individuals to buy health insurance. Given that, they argue, the entire ACA is unconstitutional.
If the Supreme Court agrees and strikes down the full ACA, Medicaid expansion would be jeopardized, Mr. Janda says.
However, justices have the alternative option of striking down only the narrow provision requiring individuals to buy health insurance. Even so, lawmakers will have to deal with the uncertainty about the Supreme Court case through most of their deliberations about Medicaid expansion, says John Pitts, a health care consultant and co-author of one of the EHF reports.
“The problem is that we probably won’t know what the Supreme Court does until very late in the [legislative] session,” he told Texas Medicine.
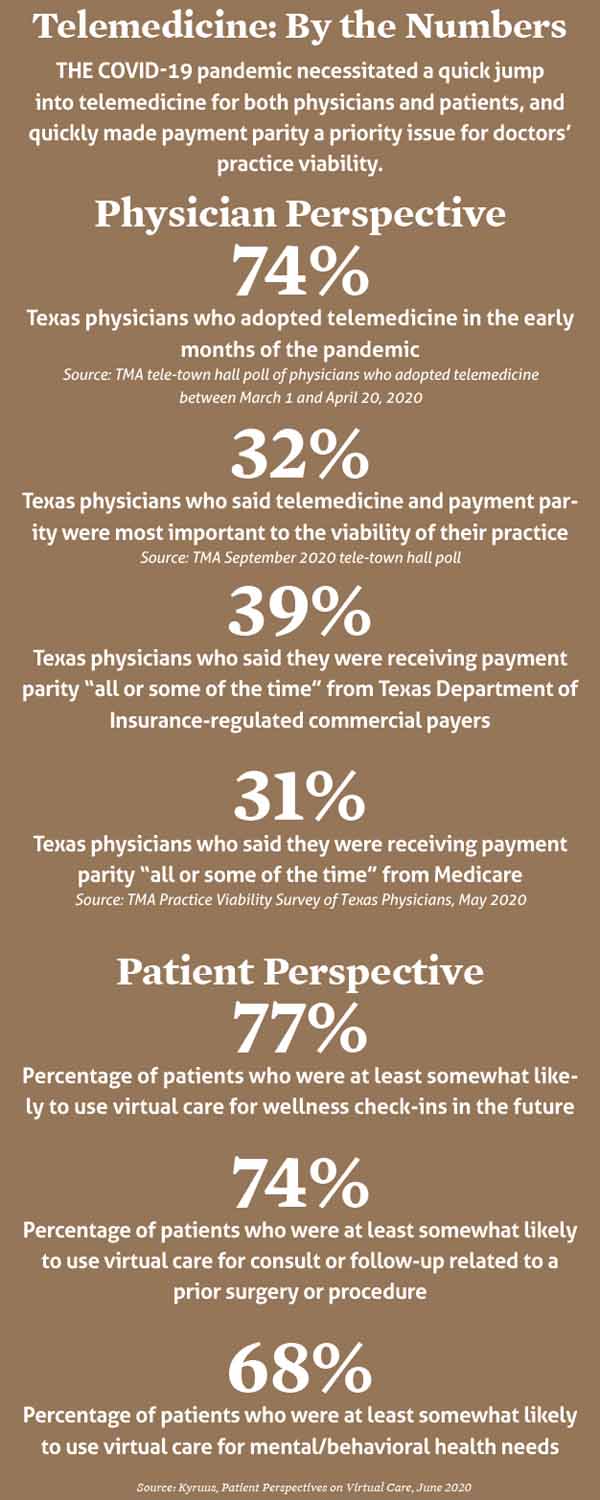
TELEMEDICINE: PROOF FOR PARITY
By Joey Berlin
The COVID-19 pandemic has been telemedicine’s ultimate proof of concept. Now, TMA hopes to take that proof to the Texas Legislature and coax the next big advancement for telemedicine in Texas: payment parity.
Early in the pandemic, policymakers at both the state and federal levels realized the immediate need for remote visits and enacted temporary rules requiring insurers to pay for telemedicine visits at the same rate as an in-person visit.
That ensured needed access to telemedicine for patients either temporarily barred or unwilling to come into the office. Patients and physicians collectively made it work, successfully implementing telemedicine at a speed many doctors never would’ve envisioned. So TMA has its sights on persuading the 2021 legislature to make payment parity a fixture.
Edinburg internist Linda Villarreal, MD, TMA’s 2021-22 president-elect, is one physician who won over not only her patients, but also herself, through her first real use of telehealth technology. “If you’d have asked me this a year ago, I’d say ‘Aaaah, no, I don’t think so. I’m not really interested in that,’” she said.
But with the pandemic surging in the Rio Grande Valley in the summertime, Dr. Villarreal’s practice responded to what she calls the “hyperdrive” need to adjust for the fear and angst that prevented patients from coming into the office. They introduced telemedicine to their patients with productive results.
“We have a large geriatric, Hispanic population with maybe bigenerational or trigenerational homes, where the grandma is there taking care of the third generation. That particular type of patient may not have been able [to adjust] as easily as the Baby Boomers, who are used to iPhones and iPads and computers,” Dr. Villarreal said. “So we did have that kind of block initially. How we overcame that is by getting their granddaughter or their grandson or their son who was at home with them to help them with the technology, whether it was an iPad, a computer, or an iPhone.”
Austin endocrinologist Thomas Blevins, MD, says while telemedicine has its limitations, they’re “far outweighed by the benefits.” His practice began using it in mid-March 2020, and it became a worthy alternative to in-person visits for diabetes, thyroid problems, and other chronic diseases. A patient with diabetes in her 70s who lives more than an hour away could see Dr. Blevins via telemedicine, and he could download and analyze data from her insulin pump. She also was able to get her labwork done near her home, allowing for “basically … a normal visit” with Dr. Blevins.
While Texas physicians had some technological and logistical difficulties in the rapid switch to telemedicine last year, the adjustments they made with their patients largely showed that remote visits could often be equivalent, value-added care. (See “The Tele-Future Is Now, July 2020 Texas Medicine, pages 14-19, www.texmed.org/telefuture.)
“The value of the visit, from my viewpoint, is in-person or not, it’s pretty much the same,” Dr. Blevins said. “If you’re talking about parity, there’s no devaluation. There’s no less value to the patient, in my opinion. There might be cases where that’s true, and some patients might perceive it that way. But the majority of people are very happy with the telemedicine experience.”
In 2017, TMA successfully backed a legislative measure that provided a framework for telemedicine in Texas, removing the requirement for an in-person meeting to establish a patient-physician relationship as long as the standard of care could be met via telemedicine. And in 2019, the legislature passed several bills advancing the new technological frontier even further, including measures that required Medicaid coverage of telemedicine and permitted telehealth treatment for substance abuse.
TMA has pushed for telemedicine payment parity for several sessions, but heavy resistance from insurers largely stymied medicine’s efforts. Other challenges have continued, such as inadequate broadband access in rural areas of Texas. Last fall, the Governor’s Broadband Development Council recommended that the legislature create a state broadband plan and study the potential development of a state broadband funding program for underserved areas. TMA President Diana Fite, MD, supported those recommendations.
If payment parity becomes reality for state-regulated plans in 2021, TMA will finally have convinced lawmakers of the position medicine has preached for several years: That a health plan should pay a contracted physician for a covered service at the contracted rate regardless of how the service is provided.
TMA Vice President for Advocacy Dan Finch says the decision on whether to provide the service by telemedicine or in-person should be up to the patient and the physician. While insurers still aren’t receptive to payment parity, Mr. Finch says the idea has drawn bipartisan support. Within the first two days of early filing in November, he noted, there had already been two payment parity bills filed, one from a member of each political party.
“Telemedicine hasn’t replaced the need for in-office patient visits,” Mr. Finch said. “But it has been a boon to practices and patient care when it’s feasible and appropriate to do it. Telemedicine can’t replace everything a physician does for his or her patients, but it can do a lot. And we’ve seen a lot of services provided by telemedicine. It’s been good from a medical standpoint. It has been helpful to many struggling medical practices trying to stay above water at a time when patient volumes are not back to what they were pre-pandemic.”
Tex Med. 2020;117(1):20-27
January 2021 Texas Medicine Contents
Texas Medicine Main Page