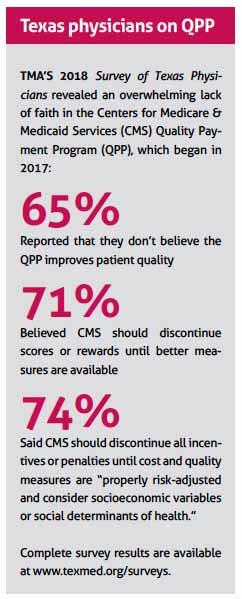
Small and solo practices already take the worst of the administrative and financial pounding the Quality Payment Program (QPP) dishes out each year.
In the Texas Medical Association’s analysis, the government’s plans for the QPP in 2020 would make the situation even harder on those smaller shops.
Since QPP’s birth in 2017, small practices have struggled with the demands and synapse-straining complexities of the program’s Merit-Based Incentive Payment System (MIPS). And TMA analysis shows the payment penalties those “have-not” practices incur fund the bonus payments earned by MIPS “haves” – often, larger practices with the resources to make the program work.
Under the 2020 changes that the Centers for Medicare & Medicaid Services (CMS) has proposed, the maximum penalties for practices who don’t hit their MIPS targets will be larger than ever. But TMA’s review shows that MIPS – despite CMS’ claims to the contrary – isn’t getting any simpler.
CMS released its proposed changes to the QPP for 2020 as part of its draft Medicare physician fee schedule – a document that amasses hundreds of pages of excruciatingly detailed rulemaking. At press time, TMA was working on a comment letter to respond to the proposal, emphasizing the need to simplify the QPP.
Austin otolaryngologist Jeffrey Kahn, MD, chair of TMA’s Council on Health Care Quality, likens the government’s approach to QPP to building a house and continuing to add on to it without knowing whether the foundation is sound to begin with.
“The concerns that many people share is that they’re now adding more penalties and raising the stakes on this in order to just say, ‘Well, we said we were going to, so we’re going to,’ without really digging into their own initial data deeply enough to see whether or not the program is making a meaningful, positive difference, and without recognizing the impact that it’s having in terms of the disparity that TMA’s research has demonstrated,” he said.
Higher targets, higher penalties
In a fact sheet it released on the QPP proposal for 2020, CMS acknowledges that clinicians have stated “the program, specifically MIPS, remains overly complex.
“Our approach for the 2020 Performance Year is to maintain many of the requirements from the 2019 Performance Year, while providing some needed updates to both the MIPS and Advanced [alternative payment model] tracks to continue reducing burden, respond to feedback that we have heard from clinicians and stakeholders, and align with statutory requirements.”
But the financial burden, at least, for falling short in MIPS wouldn’t be reduced under the CMS proposal. During the current year, practices can earn a maximum bonus or penalty of 7% of their Medicare billings based on their MIPS performance. (Because MIPS “payment adjustments” are assessed two years after a performance year, those bonuses or penalties will come in 2021.)
In the proposed rule, the maximum bonus or payment penalty practices could receive in 2022 would increase to 9%.
That might sound great if you know your practice can hit its targets. But if you’re a smaller shop, a 9% penalty could be devastating on top of your yearlong failure to meet the program’s demands.
 While these percentages were defined in the law, bonuses for top performers thus far have not been as high as originally planned. Because of factors such as MIPS being a budget-neutral program, the maximum MIPS bonus paid out this year (for 2017 performance) is 1.88%, and only 1.68% for 2020 (for 2018 performance), resulting in little to no return on investment for many physician practices. So it’s almost certain that actual bonuses for the 2020 performance year will not reach 9%. On the other hand, penalties, which are based on a sliding scale, can reach 9%; practices that are required to participate but don’t will get that penalty automatically.
While these percentages were defined in the law, bonuses for top performers thus far have not been as high as originally planned. Because of factors such as MIPS being a budget-neutral program, the maximum MIPS bonus paid out this year (for 2017 performance) is 1.88%, and only 1.68% for 2020 (for 2018 performance), resulting in little to no return on investment for many physician practices. So it’s almost certain that actual bonuses for the 2020 performance year will not reach 9%. On the other hand, penalties, which are based on a sliding scale, can reach 9%; practices that are required to participate but don’t will get that penalty automatically.
Along with the higher bonuses and penalties, the minimum score to avoid a payment penalty increases under the CMS proposal, too. This year, you needed a final score of 30 points to avoid a penalty. Under the 2020 proposal, the score you need to hold serve would be 45 points. To earn an additional bonus for “exceptional performance,” you would need a score of 80 points, instead of this year’s 75.
“Our goal is to continue incrementally increasing the performance threshold to meet the requirements established by Congress that beginning with the sixth year of the program (2022 Performance Year) the performance threshold needs to be set at the mean or median of the final scores for all MIPS eligible clinicians for a prior period,” CMS said in its fact sheet. Upping the thresholds was also “a response to the strong performance of clinicians” in MIPS in 2017 and 2018, CMS said.
The 2017 performance year featured a highly flexible, “pick your pace” approach that made MIPS participation relatively easy. And still, according to CMS, physicians in small and solo group practices averaged a MIPS score of just 43 points – significantly below large practices’ average performance of 74 points. Practices participating in a MIPS alternative payment model in 2017 averaged 87 points. (CMS has not released data for the 2018 performance year.)
“Many people would argue that in the end, because we’re not truly proving the value of this value program, we are to some degree just arbitrarily re-apportioning Medicare dollars,” Dr. Kahn said. “Essentially that is, that the people who can afford to jump through the hoops and know how to play the game are going to benefit, and the people who don’t have the resources and don’t know how to play the game as well aren’t going to benefit. But those that can’t afford to play the game aren’t necessarily providing less value in the medical services they provide.”
Angelica Ybarra, TMA’s director of clinical advocacy, says CMS “has not published any data to date that demonstrate the QPP is actually achieving its aim as envisioned by [the law] and Congress, such as improving the care and population health of Medicare beneficiaries, lowering Medicare costs, and minimizing burden on practicing physicians.”
MVPs: A new approach?
One of the major pieces of CMS’ vision for the future of the program, known as MIPS Value Pathways (MVPs), would begin in 2021. CMS claims MVPs are a new framework that will reduce reporting burden and “align and connect measures across the Quality, Cost, Promoting Interoperability, and Improvement Activities performance categories of MIPS for different specialties or conditions. A clinician or group would be in one MVP associated with their specialty or with a condition, reporting on the same measures and activities as other clinicians and groups in that MVP.”
What that means – at least, in CMS’s telling – is required reporting measures and activities that make sense.
“The goal,” CMS says in the 2020 QPP fact sheet, “is to move away from siloed activities and measures and move towards an aligned set of measure options more relevant to a clinician’s scope of practice that is meaningful to patient care.”
According to an example diagram CMS released, surgeons participating in MIPS would have to report on three quality measures instead of six. Those measures would be surgeon-specific, as opposed to the current structure of surgeons choosing from the same set of general measures as all other MIPS participants. The surgeon would report “on fewer measures overall in a pathway that is meaningful to their practice,” CMS claims.
TMA’s initial analysis, though, finds “no significant change from the current structure,” Ms. Ybarra said. In fact, TMA is concerned that MVPs give physicians less freedom and may bring more costs.
“While CMS reports MVPs would be more meaningful and reduce burden, TMA believes the administrative and cost burdens associated with program participation have the potential to increase,” she said. “For example, TMA anticipates changes to existing reporting methods, such as requiring physicians to submit data only through electronic means or registry vendors, and that updates to electronic health record systems would likely be required involving costs that vendors may pass on to physician practices. In addition, because MVPs would include predefined sets of measures and activities, physicians would lose the freedom to choose the measures and improvement activities that are most meaningful to their practices and patients.”
Participation threshold stays the same
TMA was happy to see one big piece of the 2020 QPP proposal: The low-volume threshold, which sets the criteria to exempt practices from MIPS, would remain unchanged in 2020.
As was the case this year, physicians are required to participate in MIPS if they bill more than $90,000 for Part B covered professional services; see more than 200 Part B patients; and provide at least 200 covered professional services to that patient group. If you meet one or two of those criteria, but not all three, you can opt in or voluntarily report to MIPS.
Although TMA would like to see those numbers increased to exempt more practices from the MIPS requirements, it was pleased to see those criteria stay put, as lowering the thresholds would subject more ill-equipped practices to MIPS reporting burden.
Noting the competitive disparity between the haves and have-nots in QPP “isn’t to say that there isn’t something good coming out of this program,” said Dr. Kahn. “There may be some very good things. But it’s certainly not a program that I think was designed or is working across the entire spectrum of health care. I think it may be providing some advantages in some areas, but then in other areas, like specialty care, it’s really unclear that specialists are being judged on anything that has any true value when it comes to trying to improve value.”
At press time, TMA was preparing its comments ahead of the CMS submission deadline on Sept. 27. Ms. Ybarra said TMA’s analysis of the 2020 CMS proposal was “focused on making recommendations that would support a fair and ethical program for all physicians.”
Tex Med. 2019;115(10):24-26
October 2019
Texas Medicine Contents Texas Medicine Main Page