
Dallas maternal fetal medicine specialist Emily Adhikari, MD, and Fort Worth infectious disease specialist Emma Dishner, MD, called it “the great imitator” and “the great masquerader,” respectively, for its ability to go undetected for periods.
Both also encounter confused patients unsure about where their diagnoses came from, saying many patients believe – incorrectly – that the disease has flatlined across the country.
“In the past, we nearly eradicated syphilis, so people stopped thinking about syphilis. ... We may have generations of trainees who didn’t see syphilis in training and know what it is like, so they don’t know how to recognize it,” said Dr. Adhikari, medical director of perinatal infectious diseases at Parkland Hospital and chair of the Texas Medical Association Council on Public Health’s syphilis workgroup. “It doesn’t usually cause a person to feel sick – that's a part of the trouble.”
Since beginning her career at the Texas Department of State Health Services (DSHS) in 2017 as infectious disease medical officer, Jennifer Shuford, MD, has been closely monitoring syphilis. The disease had captured the concern of the former state epidemiologist and current commissioner.
“In 2018, I had given a presentation talking about congenital syphilis cases in Texas,” just as cases began to skyrocket, she recalled. “It was interesting because when I presented the case data, I had some people say, ‘Are you sure about those numbers?’ What we have seen since then is year-over-year increases.”
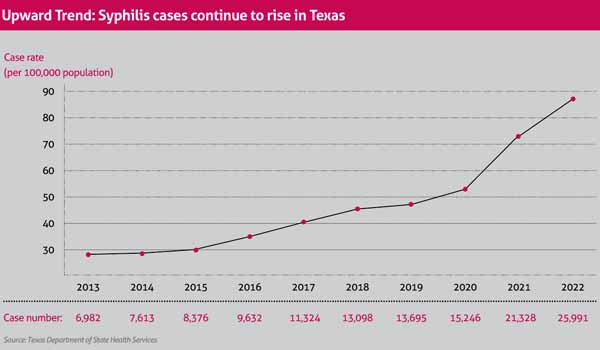
The often under-discussed disease still heavily affects Texas, giving the Lone Star State the fourth highest case rate in the nation, with cases rising 148% from 2017 to 2022, according to DSHS data. Syphilitic stillbirths rose more than 207% during the same five-year window. (See “Upward Trend,” page 45.)
The startling statistics have physicians concerned as the lack of awareness around and complexity of syphilis treatment make curbing the disease difficult.
Looking to unmask the disease and slow the epidemic, TMA’s workgroup, alongside state health officials, is taking steps to better track syphilis and to encourage education, testing, and treatment.
TMA experts also highlight the need for an all-inclusive approach from various levels of health care, including pediatricians, family and emergency physicians, and those in the infectious disease field.
The need is urgent, Dr. Adhikari says.
“In Texas, there is a disparity in syphilis diagnosis as well as outcomes related to congenital syphilis. This is multifactorial, but we think it relates primarily to disparities in access to care, stigma surrounding syphilis and substance use, and structural factors affecting health equity. In Texas we are seeing our rates rise higher than other parts of the nation.”
Dr. Shuford explains that, around the same time as her 2018 presentation, the state began ramping up surveillance of and testing for syphilis as well as monitoring trends among patients. Those changes made it possible to diagnose the disease more accurately, specifically in pregnant patients.
In Texas, three syphilis tests are mandatory throughout pregnancy visits, and positive cases of syphilis and congenital syphilis must be reported to local health authorities.
Although DSHS does not track long term children born with congenital syphilis, “we know the long-term complications from untreated syphilis in both children and adult populations. For children, it can cause a whole array of long-term health effects,” Dr. Shuford said. “This is why it is so important for adults to get diagnosed and treated before it gets passed on to babies. Kids can have immediate effects and long-term effects, and we are seeing that now with the increasing numbers of congenital cases.”
More than anything, physicians are hoping necessary attention can be brought to the disease simply by talking about it more, despite how uncomfortable it may be.
“There is a misconception that syphilis is only prevalent in people who are younger, more sexually active, and [fall into] a promiscuous subset, like sex workers. While it is more common in those populations, it exists for everyone,” said Dr. Dishner, who added that she nicknames syphilis the “masquerader” because she often treats patients who do not fit such stereotypes. “Patients come into my office with positive syphilis tests who are in long-term, monogamous relationships but never got tested prior.”
Much of the patient education she recommends mirrors that for other sexually transmitted diseases, including regular testing, use of condoms during sexual intercourse, and discussing sexual activity and treatment plans.
One recent obstacle to treatment is a shortage in penicillin production, the only Centers for Disease Control and Prevention-recommended medication for pregnant people and children with congenital syphilis, Dr. Adhikari said.
“It can be frustrating at times because syphilis is very treatable and problems arise when it remains untreated. Although physicians are not in charge of medication production, if we know patients are carrying syphilis, we can organize treatment plans.”
Physician education and resources are proving to be equally important.
Infectious disease specialists at UT Health San Antonio have introduced a new physician resource related to congenital syphilis, the Ongoing Care of Congenital and Perinatal Infections – or OKAPI – program (tma.tips/OKAPI). The free, 24/7 telehealth support system aims to assist pediatric infectious disease specialists in treating the disease, among other neonatal illnesses, and also is available to nurses, pharmacists, and infection preventionists.
Joseph Cantey, MD, is a pediatric infectious disease and neonatology specialist who helped launch the hotline with federal grant support from the Agency for Healthcare Research and Quality. At least one-third of the calls that come in are related to congenital syphilis, he says.
Syphilis “is sparing nobody. All demographics and races are affected. It is the most popular topic on the hotline because, in many areas of the state, clinics do not see it as often,” said Dr. Cantey, an on-call doctor for the hotline and member of TMA’s Committee on Infectious Diseases.
“While I may see 10 cases of congenital syphilis a week, [clinicians] in rural areas of Texas might not see one case a month. We hope to help familiarize those doctors and nurses who aren’t used to treating those types of diseases on a regular basis.
Health Reporter, Division of Communications and Marketing
(512) 370-1392