“Originally, this process wasn’t that complex, at least for me. But over the years, it has taken on a life of its own,” said Dr. Schultz, a past member of the Texas Medical Association’s Council on Practice Management Services (now the Council on Member Experience).
As the U.S. health care system shifts away from traditional fee-for-service in favor of value-based care, quality measures have become an increasingly important tool in tracking health care processes and outcomes and determining Medicare payment.
But mastering the maze of quality reporting, with its many pathways, categories, and consequences, can be elusive.
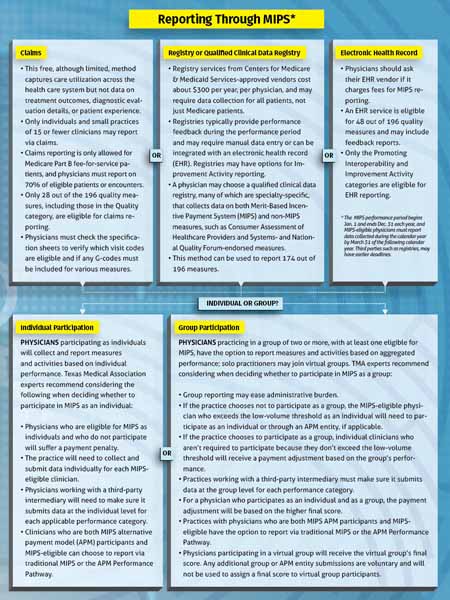
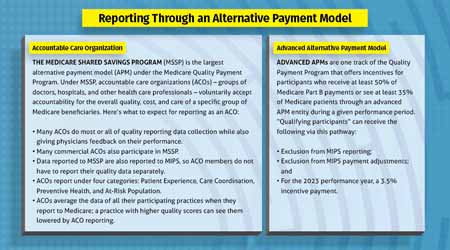
Dr. Schultz participates in and reports via the Merit-Based Incentive Payment System (MIPS), one of the pathways available under Medicare’s Quality Payment Program (QPP). Another way is through alternative payment models, which offer up to a 5% incentive payment and other rewards.
Through each of these routes, physicians get paid based on their performance across four categories, each representing a portion of physicians’ overall score:
- Quality (at least six measures), which, depending on the reporting method, may be for Medicare fee-for-service patients only or for a full patient panel (30%);
- Improvement Activities to clinical care processes and patient engagement, performed for 90 consecutive days with the entire patient panel (15%);
- Promoting Interoperability (at least nine measures) through certified electronic health record technology to support and promote the electronic exchange of health information (25%); and
- Cost of care, based on claims, with no reporting requirement (30%).
Those who choose not to participate could receive up to a 9% cut to their Medicare payments – all but forcing eligible physicians to participate, Dr. Schultz says.
“As quality reporting has become more complicated, it’s become very difficult to know which indicators I should participate in and which I shouldn’t. Right now, I’m just doing my best to report all measures that make sense to me,” he said.
For instance, more than 60% of family physicians have contracts with seven or more payers and are responsible for reporting different quality measure sets to each, according to the American Academy of Family Physicians.
“The biggest headache is that we’re without a single list of quality data across all the different payers and instead have to meet varying requirements for each,” Dr. Schultz said. “If I’m worried about checking boxes more than communicating with my patients, then the system has become a distraction from patient care.” (See “Driving the Quality Train,” page 16.)
Amid these challenges, quality reporting does have its benefits, says Tyler pulmonologist Suman Sinha, MD, a member of TMA’s Council on Health Care Quality. He participates in an accountable care organization (ACO), which has its own set of measures and reporting mechanisms similar to but separate from MIPS.
Dr. Sinha familiarized himself with the ins and outs of quality reporting to adjust to the demands and meet both his patients’ and his payers’ needs. Although he had “initial concerns” about the workload reporting would cause, he found that it became essential to treating patients with chronic illnesses.
“It does add burden,” he acknowledged. “But one of the reasons I became inspired to participate is that I saw value in how it helped keep track of patient needs. I should understand the needs of all my patients and provide the opportunity for every single one of them to get treated regularly. And I couldn’t do that without an organized approach to that population.”
Reporting options
According to QPP, how physicians choose to report data and which methods are available to them depend on:
- Whether a physician is participating as a group;
- Practice size;
- The type of information technology a practice uses; and
- The performance category a physician is reporting under.
For instance, measures under the Quality category can be reported through claims, third-party registry, or electronic health record (EHR), while measures that fall under Promoting Interoperability or Improvement Activities can be reported via some registries or EHR.
And because not all measures can be reported via all methods, individual reporting options contain benefits and drawbacks.
Once practices identify which reporting mechanisms they can use, they must ensure these options are viable for their practice, Dr. Schultz says.
“The biggest thing when deciding whether a pathway is worth it is looking at how difficult it is through your current situation,” he said. “How much work will it take to achieve that increase in reimbursement? How long will this option be viable?”
Dr. Schultz uses his EHR system to report quality measures “because of ease of use” but notes that what works for his practice may not work for others.
For Dr. Sinha and his ACO, an EHR provided a pathway to report quality measures while ensuring patients receive the care they need. Keeping in mind that not all quality measures can be reported via all methods, Dr. Sinha says having one system in place aided the process “tremendously.”
“EHRs were originally designed to optimize billing and collections,” he said. “But now they’re becoming the center point of health care after being retrofitted to care for patients, and they’re doing a reasonably good job. Many of us probably wouldn’t have made it without experts to guide us through this process.”
Quality reporting can be tricky, Dr. Sinha says.
“Physicians are busy, overwhelmed, and often burned out,” Dr. Sinha said. “But it takes these processes and steps to learn and to move us in the right direction – one where we’re paid based on the outcomes and the high-quality work that we’re really doing.”