
Physicians have not always been big fans of the Merit-Based Incentive Payment System (MIPS), one of the two participation tracks in Medicare’s Quality Payment Program.
MIPS is widely seen as an overwhelming administrative burden and an underwhelming source of payment.
But there is an aspect of MIPS that can be very helpful for physicians looking to protect electronic health records (EHRs) from errors, hacking, and similar problems, says Dallas pediatrician Joseph Schneider, MD, a former chair and current member of the Texas Medical Association’s Committee on Health Information Technology (HIT).
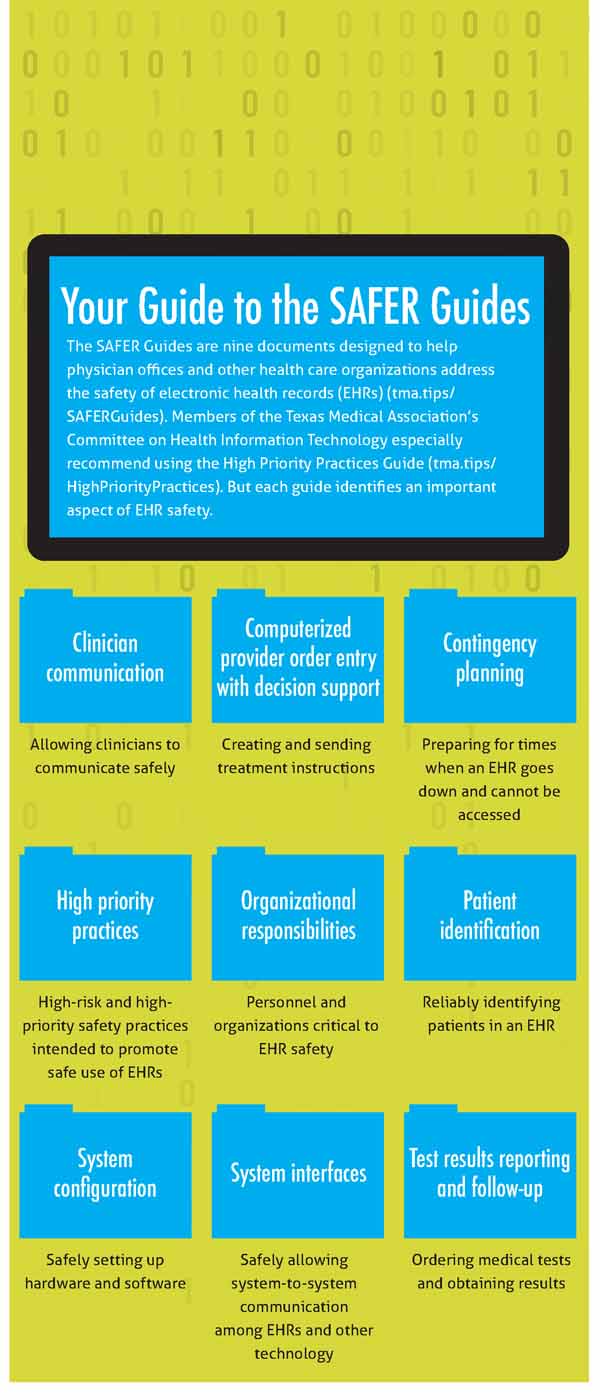
Specifically, physicians can turn to the MIPS High Priority Practices (HPP) Guide, which is part of the nine Safety Assurance Factors for EHR Resilience (SAFER) Guides, Dr. Schneider says. (See “Your Guide to the SAFER Guides, page 29.)
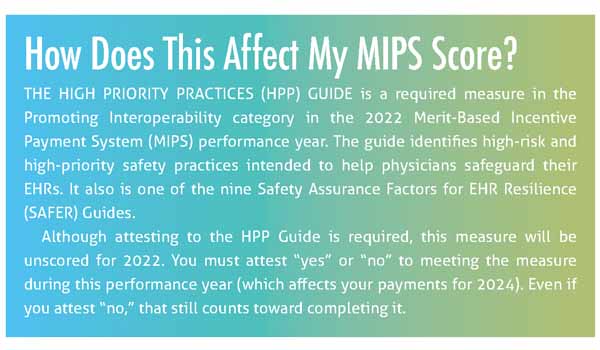
The HPP Guide is a required measure in the Promoting Interoperability category in the 2022 MIPS performance year. Completing the HPP Guide won’t affect your MIPS score for 2022, but it can help you identify high-risk and high-priority safety practices that can promote the safe use of EHRs. (See “How Does This Affect My MIPS Score?” page 27.)
“The SAFER Guides [including the HPP Guide] are a wellness or preventative tool, similar to a physical checkup,” Dr. Schneider said. “The fact that the government has decided that they don’t impact this year’s MIPS score should have nothing to do with whether you should use the guides to help prevent errors or problems, which are essentially technological morbidity or mortality.”
Physician practices typically iron out many EHR-related problems as they begin using a new EHR, says Fort Worth pediatrician Matt Murray, MD, also a former chair and member of TMA’s HIT Committee. But EHR problems never go away, and the SAFER Guides are already available and an efficient way to continue identifying those problems.
“Although EHRs have eliminated most of the old, paper-based medical record risks, they have introduced a new set of EHR-related risks that now need to be managed,” he told Texas Medicine.
There is no standard amount of time for working through the HPP Guide or other SAFER Guides because that depends on how deep a medical office explores each recommended practice, Dr. Schneider says. However, TMA’s HIT Committee recommends practices consult the guides to avoid costly and potentially dangerous errors in using their EHRs.
“A practice can, of course, not use the SAFER Guides and hope that they have covered everything important,” he said. “Or, they can piggyback off of the wisdom that went into the development of the guides and have a much better chance of not missing important safety issues.”
Avoiding errors, reducing risk
The HPP Guide covers 18 major points that physician practices should look at when assessing EHR risks. These include guidance on topics like backing up data, how to safely test hardware and software, and preparing for “downtime” – those inevitable periods when an EHR is unavailable.
The HPP Guide provides a checklist for each of these 18 points to help physicians ensure they’re appropriately using and protecting their health information technology. Each item on the checklist comes with a corresponding worksheet that describes the rationale for why the recommendation is on the checklist, as well as examples of useful practices or scenarios for that recommendation.
Dr. Murray is no stranger to the slippery ways EHRs can introduce errors into patient care, some of which are technical glitches that are hard to foresee.
“I was once involved in a situation where instructions for a child’s insulin dosing were correctly entered into the EHR discharge instructions, but when the mother received the printed instructions, there was a decimal point error resulting in a 10-times dosing error,” he said. “This error was fortunately noticed by the nurse and corrected manually. He reported this near-miss to the EHR vendor, and they also corrected the technical problem.”
But other errors are caused by humans juggling a lot of priorities in high-pressure situations, as Dr. Murray learned the hard way.
“There were times when I had multiple patient records open on my laptop as a workflow aid, but this tactic is now known to make it easier to enter orders on the wrong patient,” he said. “The first time I entered orders for an antibiotic on the wrong patient tab, it was fortunately discovered before being administered because a pharmacist inquired about the order. As a result, I changed my workflow to have only one patient tab open at any one time and have subsequently had no more similar medication errors.”
While the HPP Guide is a great place to start for avoiding errors, paying attention to all the SAFER Guides can improve a practice’s technological safety, Dr. Schneider says.
He acknowledges that taken together, the SAFER Guides may be too much for a small practice to complete all at once and recommends starting with just one – like the HPP Guide – and expanding from there as time permits. Although practices may not have time to assess everything on the checklists, using them could be a helpful activity for staff. They can divvy up various aspects of EHR security and report back on significant findings or suggestions for improvement.
Every practice can find aspects of the SAFER Guides that will benefit EHR safety and security, Dr. Schneider says.
“Classic cases that have happened are where practices are not prepared for downtimes or ransomware” in which a criminal uses malware to hold data hostage in exchange for money, Dr. Schneider said. “The SAFER Guides can help practices prepare for contingencies.”
Practices also will differ on which parts of the SAFER Guides are most useful, he says.
“It partly depends upon the skills of the technical staff as to which guide is most valuable,” Dr. Schneider said. “From my own perspective, I think the Contingency Planning Guide is the most important, but that’s just because I’ve seen [EHR] downtimes way too often.”
In other cases, some of the guidance may sound a little too obvious, but even obvious things can be overlooked, he says.
“For example, in the Clinician Communication Guide, there’s an item that states, ‘The EHR facilitates accurate routing of clinician-to-clinician messages and enables forwarding of messages to other clinicians,’” he said. “For me, that’s so basic that I might ask, ‘Why is that even a question?’ But just like the question ‘Are the fuel tanks full?’ on an airplane, there are cases where the simple things are missed.”