Stretched to the Limit
 There came a moment when all the clicking on boxes, filling out forms, and waiting on hold was just too much for Houston internist Lisa Ehrlich, MD. The time and energy spent on all of these seemingly endless tasks meant she could not give nearly enough to her patients.
There came a moment when all the clicking on boxes, filling out forms, and waiting on hold was just too much for Houston internist Lisa Ehrlich, MD. The time and energy spent on all of these seemingly endless tasks meant she could not give nearly enough to her patients.
And after 19 years in private practice, with insurance companies and the government expecting her to care for 3,000-plus patients, she was burning out.
“I was really tired, exhausted,” Dr. Ehrlich said. “I did not want to go to work in the morning. … I was stretched to the limit.”
On the outside, her practice looked like the model of success. She earned recognition from the Health Care Incentives Improvement Institute for diabetes care, for asthma care, and for using health information technology. Vitals.com — an online physician rating system — regularly gave her its Patient’s Choice Award and Compassionate Doctor Recognition.
Dr. Ehrlich and her partner employed seven billing and clinical care staff, and could have used even more help. Meanwhile, payments were diminishing and electronic health records costs were exploding. “We were drowning,” she said.
“I was forced to begin limiting the time I spent with my patients and offload communications to my staff. I was spending more than half of my time on paperwork, haggling with insurance, and regulatory box checking.”
She worried that quality-improvement programs were doing little to keep her patients healthier or to hold costs down. She chafed at the forces that transformed the medical record — her patients’ charts — from a clinical instrument into a tool to satisfy third-party payers and government regulators. She seethed at wasting time with prior authorization phone calls that took her away from her patients.
“We were, and still are, in a constant exercise that’s really designed to save the middleman money,” Dr. Ehrlich said. “It’s not for the care of the patient, and it’s not actually really saving money. It’s a tax on our practices. It’s a tax on us.”
In response, she staged her own revolution. Twenty-five years after graduating medical school, she eschewed joining forces with a big hospital system and instead reinvented her practice. Even though the personalized care model she implemented means she is accessible to her patients nearly 24/7, Dr. Ehrlich says she is happier — and saner. She’s still clicking and haggling, but on behalf of only 600 patients, all of whom she knows well.
“This arrangement has put the joy of practicing medicine and really caring for patients back in my life,” she said.
Her patients have a deeper, personal relationship with their very own physician, who is almost always on call. “This can be life-saving,” Dr. Ehrlich said, describing one case where her intimate knowledge of a patient’s medical history led her to arrange immediate treatment for necrotizing fasciitis — more commonly known as “flesh-eating bacteria.”
Or there’s the long-time patient who called her with unusual chest pains on Labor Day weekend. With his normal lab results and electrocardiogram, Dr. Ehrlich says, most emergency rooms would have released him with no further work-up.
“But I just did not like the way he looked.”
Acting on instinct, she persuaded a cardiologist to perform an angiogram.
“He ended up having a 95-percent blockage of the left main artery, which we call the ‘widow maker,’” she said. “He was admitted immediately for bypass surgery and is a healthy survivor. In my old model, I would have had a 25-percent chance of being on call that day.”
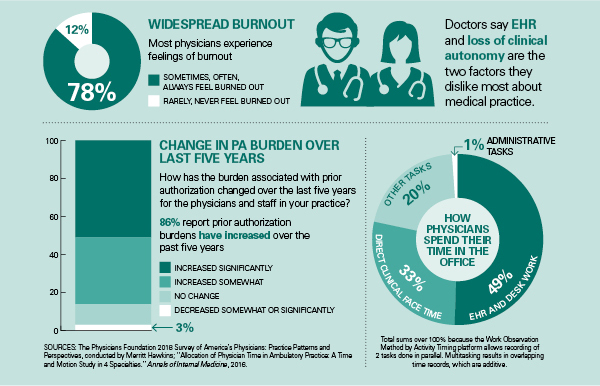
The time physicians spend with their patients is the most satisfying and, obviously, the most productive part of their day. Unfortunately, research shows, most physicians spend far more precious minutes each day sitting at computer screens, filling out paperwork, or waiting on hold with insurance companies and pharmacies. This sad imbalance is one of the leading causes of medicine’s burnout epidemic. TMA offers numerous recommendations to reduce nonclinicians’ interference in the patient-physician relationship and to streamline bureaucratic processes. Physicians currently spend only about 17 minutes of every working hour in direct clinical face time with patients. With nearly 55,000 physicians actively practicing in the state, every minute we can shave from the paperwork burden effectively translates into a 1,100-doctor increase in Texas’ physician workforce.
Health Insurance Interference
Some of the most frequent, and most irritating, intrusions into physicians’ daily lives come from health insurance companies — commercial plans as well as Medicaid and Medicare managed care organizations. Their arbitrary denials of coverage, increasing demands for prior authorization for procedures, equipment, and medications, and seemingly random changes in pharmaceutical formularies combine to eat massive chunks of physicians’ time and interfere in their ability to provide patients with the care they need.
TMA recommends that the Texas Legislature:
- Require that prior authorization reviews be performed by a Texas-licensed physician in the same or similar specialty as the physician submitting the request.
- Ensure that prior authorization approvals bind health plans to cover and pay for that service or medication and prohibit plans from denying coverage or payment after the fact based on a separate medical necessity decision.
- Require plans to automate the prior authorization process to reduce on-hold and waiting times.
- Require plans to eliminate prior authorization requirements for services, medical equipment, and medications that are routinely approved.
Prescription Drug Monitoring Program
Over the past several years, Texas significantly upgraded and improved the Prescription Drug Monitoring Program (PDMP) through which prescribers and pharmacies can look up a patient’s history with opioids and other dangerous and addictive drugs. The PDMP is an important tool in the fight against addiction and overdoses. But it is still a very cumbersome and time consuming tool for physicians to use many times each day. Electronic integration will be a process, not an event. It will take some time to realize the full benefits; ultimately, this will give physicians access to important clinical information without additional work flow interruptions.
TMA recommends that the Texas Legislature:
- Direct the Texas Board of Pharmacy to ensure that electronic health records manufacturers integrate an automatic PDMP look up into the systems they sell. This would streamline workflow in thousands of Texas physicians’ offices and reduce time-consuming interruptions to check each patient’s controlled substance prescription history manually.
- Expand physicians’ authority to delegate PDMP searches to other members of the health care team.
- Limit the initial mandate to check the PDMP before writing a prescription to Schedule II medications. (The mandate currently takes effect Sept. 1, 2019, for opioids, benzodiazepines, barbiturates, and carisoprodol in all schedules.)
Pharmacy Interference
Claiming it is part of their role in fighting the opioid epidemic, pharmacies and pharmacy chains are instituting rigid limits on the type, amount, or dosage of analgesics they will provide a patient, regardless of the physician’s prescription. Some are requiring vast amounts of patients’ clinical information before filling a physician’s valid prescription. These arbitrary limits and information requests frequently delay patient care. Fighting the limits and providing the requested medical records consume valuable time from a physician’s day.
TMA recommends that the Texas Legislature:
- Preserve physicians’ authority to prescribe appropriate medications without pharmacies interfering or overriding physicians’ valid orders.
Electronic Health Records (EHRs) and Health Information Exchanges (HIEs)
Despite the decades-old promise to revolutionize health care, electronic health records (EHRs) remain expensive, cumbersome, time consuming, and extremely frustrating for many physicians. Research shows that physicians spend only 27 percent of their day on direct clinical face time with patients, in large part because they spend nearly 50 percent of their time on electronic and old-fashioned paperwork. Numerous government and private payer programs intended to measure the quality of medical care physicians provide require volumes of data to be entered into — and later retrieved from — an EHR. Each of the programs has different rules, uses different metrics, and requires different data. Health information exchanges (HIEs) in Texas purport to enhance patient care by allowing physicians and providers to share data quickly and easily. Unfortunately, different brands of proprietary EHRs are unable to “talk” to each other without paying exorbitant fees to vendors. This barrier prevents meaningful data integration from a hospital, laboratory, or another physician into a patient’s electronic chart.
TMA recommends that the Texas Legislature:
- Align Medicaid quality requirements with other programs’, such as Medicare’s, to reduce confusion and complexity, and increase physician participation.
- Require EHR vendors to ensure their products will share data about reportable diseases directly with state and local public health agencies, and ensure those agencies have the technology to receive that data from the EHRs.
- Ensure HIEs integrate data seamlessly among physicians, hospitals, state registries, labs, and other stakeholders at no or low cost to physicians.
- Remove cost and hospital barriers that stand in the way of HIE integration between physicians and EHR vendors.
- Align all health information organizations in the state to create efficiencies for all participating stakeholders.
- Require bidirectional data sharing among health information organizations and physicians and providers that use EHRs.
Maintenance of Certification (MOC)
To renew their Texas medical license every two years, all physicians must complete at least 48 hours of continuing medical education. The vast majority of Texas physicians are voluntarily board-certified, passing a comprehensive examination after completing their residency. Certification for many is time-limited, and the certifying boards have instituted time-consuming and expensive processes for maintenance of certification (MOC), which many physicians believe offers little to no value to them or their patients. The 2017 Texas Legislature passed a law that prohibits the use of a physician’s MOC status as a requirement for doctors to obtain or renew a medical license, and bars health plans and most hospitals from requiring physicians to obtain MOC for credentialing or contracts. Many hospitals around the state have wrongly insisted that their old MOC requirements automatically remain in place despite passage of the new law.
TMA recommends that the Texas Legislature:
- Explicitly state that hospitals may not require MOC for staff privileges unless the physician members of the hospital’s medical staff affirmatively votes after Jan. 1, 2018, to do so, clarifying the 2017 law.