Houston neurologist Jerald Simmons, MD, remembers when a health plan denied payment for a routine diagnostic test for epilepsy. At the time, Dr. Simmons wasn’t sure what would cause the plan to make such a “misaligned” decision. So, he turned to Texas Medical Association experts for answers.
“The plan stated they didn’t find the test necessary, and I had no idea why,” he said. “That’s when my practice enlisted the help of TMA staff to review our medical documentation, just in case.”
Given the sheer number of patients his practice sees every day, Dr. Simmons acknowledges his practice needed expert help to understand how best to perform the often burdensome task of medical documentation, which forms the foundation of a patient’s medical record.
Between appointments, he often spends hours updating charts and documenting patient information, including changes to a patient’s condition, the evolution of care provided to meet patient needs, and supporting documentation needed for payment of services.
When payers don’t share specific reasons for denials or delayed payments, Dr. Simmons similarly has spent hours trying to discern “what went wrong” in terms of documentation. In this case, the health plan pointed to data from another study that Dr. Simmons knew, at least clinically, was not going to be helpful for this patient, yet the insurer did not explain that in its denial letter.
“You just can’t get payers to work with you. Believe me, I’ve tried,” he said. “If there’s an issue on the practice side, like missing or misfiled documentation, plans won’t tell you.”
Thankfully, TMA experts regularly meet with practices to share tips to reduce documentation mistakes, including offsetting certain tasks to qualified employees, utilizing electronic health record (EHR) features, and accurately collecting patient information, among other measures.
Carra Benson, TMA’s director of payment services, says she receives requests for documentation help from physicians “quite a bit,” often after situations like Dr. Simmons’.
“These issues can stem from a lack of communication from payers or because documentation is handled by employees who have a heavy workload and not enough time to give to ensure records have every detail accurately noted,” she said. “Correct payment is almost entirely dependent on good record-keeping. The rest comes down to navigating rules created by the government and other organizations, which is where TMA can help.”
After their review, Dr. Simmons’ practice not only discovered what was missing from the claim that prompted the denial but also received payment and obtained tips on how to avoid such problems in the future.
“This was a real help given the nature of these payers,” he said.
Lack of communication
Victoria Wright, chief operations officer at Dr. Simmons’ practice, Comprehensive Sleep Medicine Associates (CSMA), implemented some of TMA’s tips.
“We weren’t getting any kind of feedback from payers until after TMA reviewed our documentation,” she said. “Before this, we had to go off older, outdated information to make our determinations on what payers needed. And that was unfair.”
The importance of accurate medical documentation cannot be overstated, said Ms. Wright, who called record-keeping the “backbone of patient care.” But without guidance, her practice management staff struggled to keep up with changing health plan policies and a lack of communication from payers.
The problem also led some CSMA physicians to struggle to receive preauthorization exemptions, or “gold card” status, because of a void of information about what documentation was needed.
The most recent publicly shared survey results from the Texas Department of Insurance (TDI) show only 3% of physicians and health care professionals have received gold cards. This is likely due to the current eligibility threshold, which requires physicians to submit a minimum of five eligible prior authorization requests for a particular health care service within the six-month review period.
Ms. Wright believes it’s hard for physicians to meet that threshold when payers are “quick to deny and slow to respond” about what they need from prior authorization requests.
“It’s a very complicated process,” she said. “Health plans don’t teach you the secret handshake. They don’t make prior authorizations easy, which means it’s not easy to get that gold card.”
This is in spite of TDI rules that state health plans have a responsibility to notify physicians if they have been granted or denied a gold card, Dr. Simmons said.
“Physicians are following the rules to get the gold card but are then blocked at the last minute by [prior authorization] denials for reasons not communicated in the beginning.”
TMA’s help
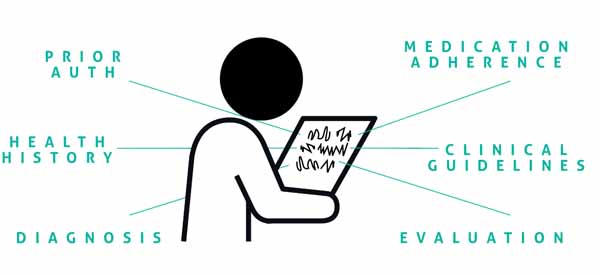
Ms. Benson recommends practices stay informed on proper medical documentation procedures to ensure accuracy and relevancy. These include:
- Communicating the patient’s past and present health information and including any medical treatment received from other clinicians. Documentation on treatment options and the physician’s thought processes in determining diagnosis or best treatment recommendations should be included.
- Using an EHR that incorporates multiple aspects of practice management, including documentation features that streamline reporting and billing.
- Training staff on clinical guidelines through various strategies, like creating groups of “super users” who take advantage of vendor training and then provide internal instruction to clinicians or office staff.
- Documenting current patient behavioral trends and intervention outcomes, such as a refusal to take medications or nonparticipation in physical therapy. In addition, records should have evidence of ongoing monitoring of the patient’s clinical condition with improvement or lack thereof documented with each visit.
- Implementing an intuitive user interface with a low learning curve to minimize the time team members spend documenting evaluations, giving them more time to focus on making patient visits more engaging.
Proper documentation is essential to efficient claims processing and timely payment, Ms. Benson emphasizes.
From there, she recommends physicians regularly undergo an internal audit to ensure all practice management procedures are followed. By doing so, practices can provide a strategic, proactive method to mitigate risk and fraud while making sure that their practice stays in compliance.
An internal audit can help:
- Improve controls, compliance, and financial operations of a practice or health care organization;
- Assess, analyze, and improve patient care and internal processes;
- Identify areas that need improvement to boost patient safety;
- Identify and address faults in compliance programs; and
- Document compliance efforts for the purposes of dealing with auditors or regulators when necessary.
Dr. Simmons said many of his practice’s denials have “disappeared” after implementing some of these documentation practices. Because of that, he remains hopeful that documentation will become easier.
“It feels like health plans change the goal post every year, but TMA specialists found a way to navigate that complex system,” he said.