
San Antonio radiologist Zeke Silva, MD, recalls the day Texas passed its groundbreaking “gold card” law in 2021, the first of its kind in the country, reducing prior authorization burden for Texas physicians and diminishing delays in patient care.
“It was a momentous achievement,” said Dr. Silva, a member of the Texas Medical Association’s Council on Legislation who worked with lawmakers to achieve the reform. “The law exempted physicians who consistently meet prior authorization requirements from ongoing burden and allowed those physicians to spend more time with patients. It was a win for Texas physicians and Texas patients.”
In his practice, for example, prior authorization improvements have expedited treatment for patients with specific care needs. Previously, Dr. Silva says, health plans would deny necessary medications because of a lack of knowledge rather than true clinical oversight.
“In one particular case, the health plans were denying women medications that they thought were only prescribed to men, despite my insistence that that was not the case,” he said. “This denial was a huge frustration.”
Texas’ gold card law has reduced such cases and has begun inspiring other states to introduce similar legislation. But Dr. Silva still hears from colleagues that further changes are needed to implement the gold card law as intended.
The Texas Department of Insurance (TDI) reports that only 3% of physicians and health care professionals have received gold cards because of the current eligibility threshold, which requires physicians to submit a minimum of five eligible prior authorization requests for a given health care service or medication within the six-month review period.
“Two years on, the law has exposed persistent hurdles to the health care system and has become a testament to physicians’ enduring challenges when dealing with prior authorization,” he said. “Frankly, by passing this law, we told insurers, ‘Enough is enough.’”
Leading the way
Physicians have long objected to onerous prior authorization requirements that often delay patient care. The Texas gold card law was introduced as a legislative response to those frustrations – and medicine’s push for improvements seems to be paying off.
On Sept. 1, UnitedHealthcare (UHC), the country’s leading health insurer, eliminated prior authorization requirements for certain procedure codes across many of its national plans, including its Medicare Advantage, commercial, Oxford, and individual exchange plans.
The change is expected to reduce overall prior authorization volume by 20% and is part of an effort to “simplify the health care experience” for patients and clinicians, according to the payer’s Aug. 1 announcement. The insurer also stated it plans to implement a national gold carding program next year.
Cigna Healthcare followed suit, removing nearly 25% of medical services from prior authorization requirements, representing more than 600 codes. This includes 100 surgical codes, nearly 200 genetic testing codes, and codes for medical equipment, prosthetics, and other services.
“With this update, prior authorization now applies to less than 4% of medical services for most Cigna Healthcare customers,” Cigna said in an August press release.
Meanwhile, Medicare Advantage (Part C) and prescription drug (Part D) plans have begun streamlining prior authorization requirements by allowing prior authorization approvals to remain valid for as long as medically necessary.
Dr. Silva says these changes would have “likely stalled” without the gold card’s passage two years ago.
“These improvements speak to the gold card’s legacy,” Dr. Silva said, and have the potential to ensure timely access to necessary medical care, especially for those with chronic conditions and complex needs.
Texas’ law also laid the groundwork for additional TMA-backed state reforms passed this year, namely House Bill 755 by Rep. Julie Johnson (D-Farmers Branch), which restricts insurers from requiring more than one prior authorization request annually for certain drugs prescribed to treat patients with an autoimmune disease or certain blood disorders.
“The bill has the potential to bring relief to those previously left in the lurch due to prolonged authorization processes. And, as in most cases, previous legislation paved the way for changes such as these,” Dr. Silva said.
Odessa allergist Vivek Rao, MD, says the gold card law made a “difference in the way the payers are behaving,” and the American Medical Association alternate delegate hears testimonies from colleagues in other states on how the law sent ripples in prior authorization reform.
“The situation today would be much worse if it were not for TMA advocacy,” Dr. Rao said. “Speaking with colleagues in other states, it seems what we did here in Texas inspired other states to follow suit.”
According to a February 2022 America’s Health Insurance Plans (AHIP) survey, prior authorization exemption practices by insurers increased in the year after Texas’ gold card law was enacted. Industry wide, nearly six in 10 plans used gold carding for medical services in 2022 (58%), compared with slightly less than a third in 2019 (32%), before Texas’ gold card’s passage.
Moreover, a high number of health plans that responded to the survey found gold carding successfully streamlined the prior authorization process for prescription medications and medical services like genetic testing, elective inpatient surgical services, and high-tech imaging. This was done by using electronic prior authorization, waiving or reducing prior authorization requirements for certain patients to promote continuity of care, and selectively waiving requirements for “high performing” physicians via gold carding, according to AHIP.
Health plan respondents also reported improved physician satisfaction and reduced administrative burden (46% each), and almost a quarter said patient safety was stable or saw improvement (23%).
Varied implementation
Not all physicians are feeling those benefits.
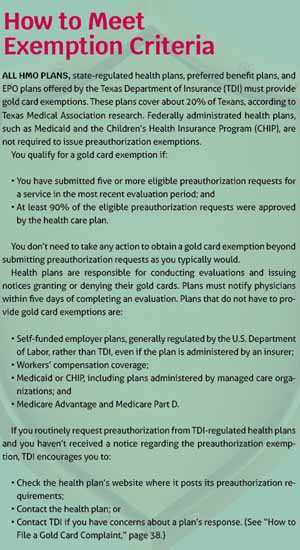
Although TDI rules state it is the health plan’s responsibility to notify physicians if they have been granted or denied a gold card, Houston neurologist William Gilmer, MD, a member of TMA’s Council on Constitution and Bylaws, sees a lack of communication from payers as a barrier in his practice. (See “How to Meet Exemption Criteria,” page 36.)
“I am thrilled that we passed the gold [card] law and that it continues to encourage change across the state,” he said. “But my practice has not been contacted by any insurance carrier to discuss gold card status. It’s almost like [insurers] don’t want us to know we’ve qualified for exemptions.”
Dr. Gilmer believes increased collaboration between physicians and health plans would streamline authorization criteria and improve communication – but he admits he’s “not holding his breath.”
“Gold card is great, but it doesn’t fix everything,” he said. “And addressing persistent prior authorization issues is a fight that physicians will be fighting for a long time.”
While gold card laws have aimed to standardize the prior authorization exemption process, implementation varies among insurers, and physicians still report care delays caused by prior authorization, according to a December 2022 survey by AMA.
Roughly 80% of physicians reported the number of preauthorizations required for prescription medications and medical services has increased over the past five years. An overwhelming majority of physicians (89%) reported that prior authorization requirements interfere with continuity of care.
“Inconsistencies in interpretation and execution continue to pose problems for physicians,” Dr. Rao said. “And many payers maintain harsh eligibility requirements. Physicians must still navigate a maze of guidelines, which leads to frustration and delays.”
Dr. Rao also stresses that TDI’s rulemaking heeded only some of TMA’s recommendations for implementing Texas’ law as written.
“When the [gold card] legislation became law, I was extremely optimistic about how that would impact my practice, and I think the law was well written,” he said. “However, during the rulemaking process, insurers were able to make alterations to the law so that it did not function the way it was expected, and on top of that, TDI incorporated new [peer review] conditions that could delay access to care and contributed to administrative burden.”
Thanks to TMA advocacy, TDI lowered the number of prior authorization requests necessary to earn a gold card to five. Although TMA lobbied for no minimum number of requests for initial granting or denial of an exemption (consistent with the legislation, which contained no minimum), the change represents a significant improvement over TDI’s proposed rules, under which physicians would have had to earn approvals on at least 90% of at least 20 prior authorization requests on a given service over a six-month period.
TDI’s rules also accord with TMA’s advocacy in other areas, including:
• Requiring health plans to describe in denial notices how to appeal the decision and file a TDI complaint; and
• Allowing physicians to specify a particular email or mailing address for notices regarding prior authorization exemptions, denials, and recissions.
However, while the law mandated that peer-to-peer calls prior to an adverse determination must be conducted by a physician licensed to practice medicine in the state in the same or similar specialty as the physician who requested the service – an interpretation echoed by the bill author’s/sponsor’s statement of intent – the final rules allow physicians with an administrative license (rather than a full medical license) from the Texas Medical Board to fill this role.
An ongoing fight
TMA tried to reverse this change during the 2023 legislative session to increase oversight when such reviews were arbitrary or without medical basis, but medicine’s advocacy was met with stiff opposition from health plans. “We tried to point out that this really is the practice of medicine for which accountability is necessary,” Dr. Silva said. Meanwhile, new health plan programs have the potential to undo certain gains made by the 2021 law.
TMA also supported House Bill 4343 by Rep. Greg Bonnen, MD (R-Friendswood), which would have expressly stated that no minimum threshold applied and strengthened oversight by requiring insurers to report their gold card results to TDI, among other provisions. The bill failed to advance out of committee, but TMA remains focused on burnishing the gold card law heading into the 2025 session.
Dr. Rao believes that, while recent insurance gains speak to payers’ willingness to work with physicians, other evolving practices show a startling “lack of understanding” from health plans of the burden prior authorization causes.
For instance, TMA recently voiced opposition to UHC’s “advance notification” pilot program, requiring early notification and the submission of substitute documentation for certain gastrointestinal procedures, and to a burdensome billing policy by Cigna requiring additional documentation for routine, minor procedure claims.
“It’s always one step forward, two steps back with payers,” Dr. Rao said. “They’ll concede to change only to implement another burdensome policy right after. I want the gold card law to flourish, but these changes make it hard to see a reduction in my prior authorization burden.”
TMA continues to lay the groundwork for gold card fixes and build support for adjustments likely to be handled by TDI through future rulemaking. Under the guidance of the Council on Socioeconomics, TMA also has resumed its in-person meetings with major Texas payers to discuss prior authorization, gold carding, and other payment policy issues after the meetings were switched to phone or Zoom during the COVID-19 pandemic.
“This will remain a goal of ours in future legislation,” Dr. Silva said. “At the end of the day, we want physicians who are doing the right things to take care of patients without delay.”