In the months before COVID-19 reached Texas, physicians say there were rumblings.
“The first thought is: ‘They better get a handle on this, or we’re going to hit a SARS situation,’” said David Fleeger, MD. The Austin colon and rectal surgeon was serving as TMA president when the pandemic began in March 2020. “It just kept coming and coming faster and faster.”
Approaching the end of his presidency, he braced for impact as he heard horror story after horror story. “It became apparent to us that we were going to need to gear up.”
Once the city of Austin shut down, Texas Medical Association Chief Executive Officer Michael Darrouzet knew organized medicine needed to start acting.
Having been through earlier public health crises, the former Dallas County Medical Society executive knew the strength of organized medicine was needed more than ever.
And that strength goes way back. After the Spanish flu hit in 1918, TMA’s leaders at the time had the foresight to create a bylaw provision that gave the Board of Trustees emergency power to function as a Disaster Board and assume certain responsibilities of the House of Delegates, such as elections and decision-making. When the COVID-19 pandemic hit, TMA swiftly invoked that provision.
Other first steps were informed by Mr. Darrouzet’s experience with the nation’s largest West Nile virus outbreak in summer 2012; the national Ebola crisis in 2014; and multiple hurricanes: Follow a standard emergency response, gather great minds, and communicate often.
Thus, TMA’s COVID-19 Task Force emerged. The effort to pool resources continued with the formation of the Health Care Industry COVID-19 Strike Force. The coalition of major health care associations in the state and Texas’ university systems went on to advise state leaders and advocate for physicians.
A crucial tenet of coordinated communication among these groups was TMA’s twice-daily Zoom calls, open to the entire TMA Family.
“I learned that that’s how you handle a crisis,” Mr. Darrouzet said. “You meet in the morning and the afternoon. How did the day go? What do you need tomorrow? Okay. Now, it’s the morning. What do you need today? How did it go? What do you need tomorrow?”
What physicians needed, especially those in private practice, was to keep business afloat.
But with personal protective equipment (PPE) in short supply, keeping medicine’s doors open would prove tough. “As [the stockpile] started to disintegrate, the calls started coming in,” Mr. Darrouzet said. “Doctors were saying, ‘I have to bring my own mask to the hospital.’ Nurses were saying they were hiding them and locking them in closets.”
It was time to go to the state. Thanks to the strength of the relationships TMA had built over the decades, the association got leaders’ attention.
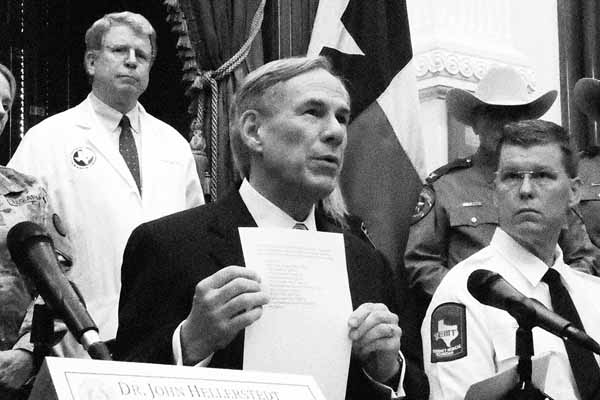
Dr. Fleeger and Mr. Darrouzet set out to the state’s Emergency Operations Center for a conversation with John Hellerstedt, MD, then commissioner of the Texas Department of State Health Services. But even a face-to-face urgent message – that medicine could not function without PPE – didn’t change the reality.
Then, about a month after TMA first met with state leaders, Mr. Darrouzet received a call from John Zerwas, MD, The University of Texas’ executive vice chancellor for health affairs. Gov. Greg Abbott had appointed Dr. Zerwas to his Supply Chain Strike Force in March, and now, Dr. Zerwas had a question: Of Texas’ 100 million-mask order, how many does TMA want?
Texas physicians could safely take a breath once PPE arrived. But distributing the materials required another big push from TMA and the strength of its network of county medical societies.
“There really wasn’t [an existing] system to disseminate PPE,” said Dr. Fleeger, who received TMA’s Distinguished Service Award in 2022 in part for his PPE work. “That was one of TMA’s shining moments: when they stood up and said they would take that on. TMA took the bull by the horns and did something that the state wasn’t prepared to do.”
The ensuing effort, spearheaded by TMA’s information technology team and coordinated through county medical societies and the Health Care Industry COVID-19 Strike Force, resulted in creation of the TMA PPE Portal.
Physicians could now request allocations of PPE directly from TMA. Those requests would then be routed through the county medical societies, which Dr. Fleeger says stepped up to the challenge readily. Larger metropolitan areas could receive shipments directly, but TMA faced yet another obstacle when it came to the 191 Texas counties considered rural. If the county couldn’t receive the shipment directly, where would the PPE be stored?
In the parking garage at TMA headquarters in Austin, it turns out. “One 18-wheeler after another,” Mr. Darrouzet said.
To move PPE requests from the garage to counties, TMA required one cost: the price of FedEx shipping.
“That, to me, will go down in history as one of the best things that TMA ever did: protecting our physicians,” said E. Linda Villarreal, MD, TMA’s 2021-22 president. “Very, very few physician offices closed during the pandemic.”
The science of good communication
Unfortunately, the triumph of getting PPE to physicians was counterweighed by an increasingly distrustful and fatigued public by the time Diana Fite, MD, an emergency physician in the Houston-Tomball area, took over as TMA president from 2020 to 2021.
Public faith in medicine certainly changed after 2020, and so did health care workers’ morale.
“At the first part of my presidency, we had certainly a lot of people who were very interested in masking and staying in place and not being around other people and trying to protect others. But as the year wore on, that changed, people got tired of that,” she said.

It was an unusual presidency for Dr. Fite, who was installed by the Disaster Board and a small group of TMA leaders at an intimate in-person event and a dramatically scaled back business session of the House of Delegates. For this first time in recent memory, the TMA president was unable to travel to visit peers in their home counties. Yet business was able to carry on virtually for the first time.
Dr. Fite may have spent her presidency giving addresses and attending meetings via Zoom – sometimes from a side office of the emergency room where she practices – but it was a vantage point that put her up close to the tragedy of the pandemic and hearing physicians’ needs.
“[I heard] heartbreaking stories of not just the deaths, but all my colleagues who would talk about how their spouses didn’t even want them to come home because they were so afraid of them bringing [COVID-19] to the children,” Dr. Fite said. “The anguish of all the nurses and the critical care physicians … [who] would sometimes reach a point where there's just nothing else to do except watch someone go ahead and die. And they were so tired.”
Her virtual platform and the strength of TMA’s reputation also gave her worldwide exposure in the media to convey the importance of science: At a time of public confusion, Dr. Fite conducted hundreds of interviews during her presidency, and a risk chart created by TMA’s COVID-19 Task Force went viral and was translated into multiple languages.
The pandemic certainly opened the door wider to anti-science sentiments. But it also provided an opportunity for TMA to step in with factual, pragmatic examples of the effectiveness of safety measures, says Mr. Darrouzet. County medical societies could then apply that information to their communities.
And TMA was there to help physicians figure out how to transition quickly to telemedicine to keep seeing patients and stay afloat.
“Physicians could actually see patients in their environment. They could get a lot of insight and take care of their patients better,” Dr. Fite said.
By the time Dr. Villarreal assumed the TMA presidency in 2021, she could take advantage of a dip in COVID cases as vaccines became available, in-person visits resumed, and some rays of hope appeared.

As she traveled around to county medical societies and medical schools as TMA presidents typically do, Dr. Villarreal was able to communicate some of that hope at a critical time: Physician burnout was reaching an all-time high.
It wasn’t until Dr. Villarreal switched to wearing only a mask and shield at the office after a year of 40-hour weeks in full PPE that she realized the cost she’d silently been paying.
“In a year’s time of having to do that every day, I experienced a depressive event,” she said. “I did not realize that had been going on in my head all that time. As physicians, we do what we do; and we do it until we don’t have to do it anymore. That’s what we all did.”
Acknowledging and embracing the depression she experienced helped her personal growth, she says.
Dr. Villarreal calls the PPE Portal TMA’s crowning achievement of COVID-19, but runner-up is the association’s response to physicians’ mental health erosion and burnout – a phenomenon that preceded the pandemic but certainly was exacerbated by it.
The result was TMA’s renewal of its commitment to put physicians’ well-being at the forefront with its Wellness First initiative and arrangement with Anticipate Joy – which provides confidential, online counseling services to physicians and their immediate family.
Going forward, looking back
There is no happily ever after to COVID-19. U.S. Secretary of Health and Human Services Xavier Becerra renewed the COVID-19 public health emergency for an 11th time this January, amid climbing numbers of omicron subvariant XBB.1.5. Anti-science sentiments persist, and some practices are still struggling financially.
But Drs. Fleeger, Fite, and Villarreal agree the difference between now and in the future is what medicine has learned over the past three years.
Disaster protocols were refined. Medicine made leaps and bounds in patient care with telemedicine. Distance communication also has improved how organized medicine conducts business. (See “A Resolution’s Journey Through the House of Delegates,” page 16.) And the medical community has banded together even more closely for moral support.
“As far as seeing what the Texas Medical Association could offer to physicians in Texas, we just shined,” Dr. Fite said.
Dr. Villarreal praised her colleague Dr. Fleeger, whom she called “the right guy” for the TMA presidency during the pandemic’s onset.
“God knew what he was doing. Who would have thought? Dr. Fleeger was the right person at the right place at the right time, and for that I will always be so thankful,” she said.
“It really was a very proud moment for the organization to be able to do as well as it did,” Dr. Fleeger said. “[TMA] honestly accomplished what needed to be accomplished that other organizations couldn’t. And I think we’d all be very proud of our TMA for having accomplished that.”