
The future of Texas medicine isn’t built on the strength of free agency. It comes from homegrown talent. Higher education is the farm system – the pipeline through which the state stockpiles and develops that talent.
So, when the Texas Legislature heeded Texas Medical Association advocacy earlier this year and fully funded the state’s Graduate Medical Education (GME) Expansion Grant Program, it was one of the most important moves to ensure Texas medical students will enter the big leagues in the Lone Star State.
“The most reliable metric for practice location, when you’re fully trained and in practice, is where you do your residency,” said Amarillo family physician Rodney Young, MD, of Texas Tech University Health Sciences Center (TTUHSC). “Financially, it’s bad business for the state to open a bunch of new medical schools, graduate a bunch of new doctors, but not have GME positions that are available in an appropriate ratio to make the choice to train in Texas an option. We do not want to be a net exporter of doctors.”
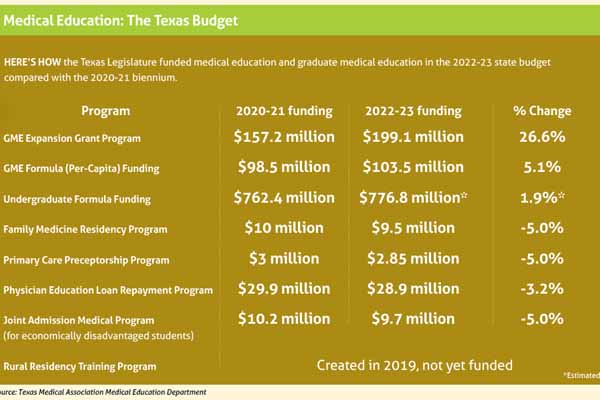
The $199.1 million for GME wasn’t the only budget bright spot for the future of Texas medical education. There were smaller victories in the 2022-23 budget as well, including an unexpected amount of money that will provide a modest bump in per-resident, or GME formula, funding to help Texas medical schools with faculty costs.
Although the push for GME funds grabbed a lot of attention during this year’s regular legislative session, TMA Associate Vice President for Medical Education Marcia Collins notes that the legislature invests a whole lot more beyond that to educate medical students. Lawmakers held the line on formula funding for medical students and gave a slight bump to overall undergraduate funding over the next two years.
With 15 medical schools now dotting the state, including six that have opened since 2016, lawmakers are demonstrating a financial commitment to the state’s future physician workforce, Ms. Collins says.
“We’re a big state, and we’re growing medical schools, so that number obviously keeps growing as well,” she said. “And the state is stepping up.”
Medical education funding wasn’t without some disappointments this year, though. Several TMA-supported programs were subject to cuts in the 2022-23 budget. They include the Physician Education Loan Repayment Program, which entices physicians to practice in rural and underserved areas by alleviating their school debt. That program already faced a funding crunch before this year’s session and stopped accepting new applicants beginning in September 2020.
“Extremely important” investment
Recent graduates like Vamsi K. Potluri, MD, know the value of giving medical school funding and GME their full due. Now a surgery intern at The University of Texas Medical Branch (UTMB) at Galveston, Dr. Potluri is a San Antonio-born, Austin-raised product of UTMB’s class of 2021. Although he had a built-in predilection to stay in his home state for medical school, that wasn’t the deciding factor.
“I was just more familiar with the medical schools [in Texas],” said Dr. Potluri, a former medical student member of TMA’s Board of Trustees and now the resident representative on the Board of Directors of TEXPAC, TMA’s bipartisan political arm. “But I did consider medical schools outside of the state, and one of the biggest [factors] for me to stay in Texas was that medical education is significantly cheaper here if you’re an in-state student in Texas, compared to other states. That played a huge role, absolutely.”
Full funding of the GME expansion grant program for 2022-23 wasn’t a given, particularly when the state’s revenue situation looked bleak in the early months of the pandemic in 2020. But Comptroller Glenn Hegar’s financial outlook improved significantly just before session began. Once the legislature got into the details of budget work, TMA advocacy helped ward off a competing proposal in the House of Representatives that would’ve left GME funding well short.
Instead, with the full $199.1 million, the state can maintain the target ratio of 1.1 GME slots for every medical school graduate.
“Texas is a large state with many rural communities. There’s a huge shortage of physicians, especially now in the COVID era when health care workers are both understaffed and overworked,” Dr. Potluri said. “Continuing to invest in graduate medical education is extremely important for the health of the state.” (See “An Overworked Force, ” page 30.)
In the last days of budget negotiations, legislators added $5 million to the funds it contributes to the faculty costs for training residents. Those funds go only to the medical schools and are separate from the GME Expansion Grant Program, which does not cover faculty costs. The funds are distributed on a per-capita basis, and the recent healthy growth in residency positions meant the funds did not spread as far as before. If the legislature had not added the $5 million for the program, the amount allocated for each resident would have dropped. (See “Medical Education: The Texas Budget,” below.)
“It’s not a lot of money when you look at how much that formula got increased, but more is more,” TMA Associate Director of Legislative Affairs Michelle Romero said. “And more is [especially] more during a difficult budget session when you’re trying to not increase funding … but you stay committed to medical education.”
That commitment of state funds can be the most – or only – stable revenue source a residency program has. Over the years, Dr. Young’s family practice at TTUHSC had put together a program of 10 annual residency positions through what he calls “a quilt … of funding sources” that included state and federal funds, rural hospital entities, and other monies. This year, after the loss of key external funding, his practice cut the program to seven slots.
“We believe strongly in the mission of training primary care physicians for Texas, particularly in our case for West Texas and for rural areas. We have a track record in that regard and a strong training program. We feel like we can offer [residents] an excellent experience, but we do need to be able to keep the lights on,” Dr. Young said. “And since we care for a disproportionate share of patients that are not as well-funded as other populations, it’s hard to do it through patient care revenues alone.”
If the Texas Higher Education Coordinating Board opens up additional grant funding spots when it begins taking applications for new GME positions, Dr. Young said his practice would seek one out “to try to help recover some of what’s been lost.”
Similar to GME formula funding, last-minute budget negotiations resulted in an additional $18.9 million for per-capita medical student funding. By TMA's estimate, state support for medical education will total about $777 million over the two years. Per student per year, the state will spend $45,733, or almost $183,000 over four years.
“We don’t want to pump $200,000 into somebody and then have them go out of state to do their residency and never return,” Dr. Young said. “Other states have that vested interest as well, but you want to have a good supply of GME opportunities close to home to make it easy to stay here.”
Key program on hold
While GME funding is in good shape for the next two years, other valuable pieces of the medical education tapestry have taken hits ranging from discouraging to serious.
The final budget also cut three programs by 5% each: the Family Medicine Residency Program ($9.5 million allocated for 2022-23), the Primary Care Preceptorship Program ($2.85 million), and the Joint Admission Medical Program ($9.7 million). The Rural Resident Training Program, established in 2019, has yet to be funded.
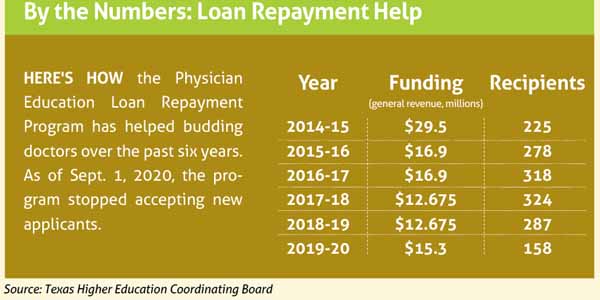
The state’s Physician Education Loan Repayment Program, which has overseen a symbiotic relationship between indebted physicians and underserved Texas communities for more than 30 years, has stopped taking new applicants. Although the program did so beginning Sept. 1, 2020, a 3% cut to its funding this year didn’t help its cause.
The program, established through legislation in 1985, assists primary care physicians with medical school loan debt in exchange for the physician serving a four-year term in a health professional shortage area (federally defined as a region with a population-to-physician ratio above 3,500-to-1). In 2009, the legislature gave the loan repayment program a dedicated funding source through a change in the state’s smokeless tobacco tax.
It offers incrementally rising amounts of loan help for each year the physician serves, currently offering up to $60,000 for the fourth year (or 34% of a loan balance under $180,000). Ms. Collins, TMA’s associate vice president for medical education, says rural, underserved communities consider the loan repayment program one of their most valuable recruiting tools.
Tom Banning, CEO of the Texas Academy of Family Physicians (TAFP), called it “hugely successful.”
Unfortunately, he added, “the legislature decided to shift priority and shift funding away from that.”
At press time, TAFP was hoping the legislature’s anticipated special session for October – in which lawmakers are expected to distribute $16 billion in federal COVID-19 relief money – would lead to funding restoration for the loan repayment program. If funding doesn’t return, Mr. Banning says it would limit the tools Texas has to put physicians in communities that need them.