
As a public health problem, obesity – both in Texas and in the U.S. – isn’t going away. But fresh perspectives on the problem are helping physicians address it.
Contrary to the misunderstandings of many people, including physicians, obesity is not “a character flaw,” says Houston gynecological oncologist Lois Ramondetta, MD, a member of the Texas Medical Association’s Council on Science and Public Health.
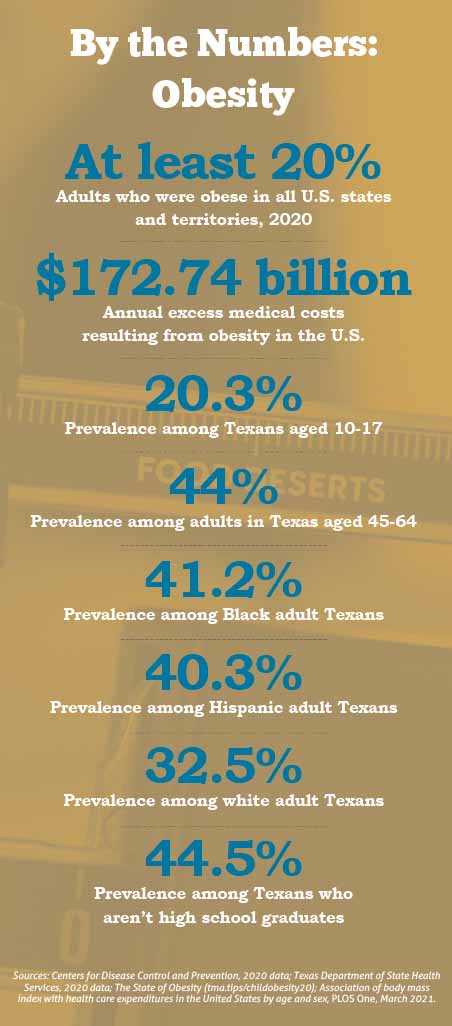
In fact, it has long been considered a chronic disease. And as an epidemic and risk factor for a host of chronic diseases – including type 2 diabetes, heart disease, asthma, and sleep apnea – it’s a health problem that is costing the U.S. more than $172 billion in excess medical costs per year.
“Early on [in my career], it definitely seemed like the answer to losing weight was always, ‘Exercise more, eat less.’ And that is not the solution for a lot of people,” Dr. Ramondetta said. “Unfortunately, the deeper you get into the obesity syndrome, the harder it is to do those things. It is a really complicated thing.”
Today, population health advocates understand one of medicine’s newest points of focus – social determinants of health – to be a major driver of obesity. Tackling the adverse effects of those nonmedical factors – for example, lack of physical access to healthy food or the financial means to buy it – is considered paramount. The COVID-19 pandemic also laid bare these impacts as obesity proved to be a significant factor for severe illness from the disease.
While the book on obesity’s root causes continues to be rewritten, philosophies on how physicians and medical schools should broach the topic are also undergoing a shift.
Still, how much physicians should directly address weight with a patient is an ongoing conversation, and source of “tension” across the medical community, says Austin internist James Marroquin, MD. He is an assistant professor in the department of medical education at The University of Texas at Austin Dell Medical School, which teaches its students sensitive conversation skills regarding obesity.
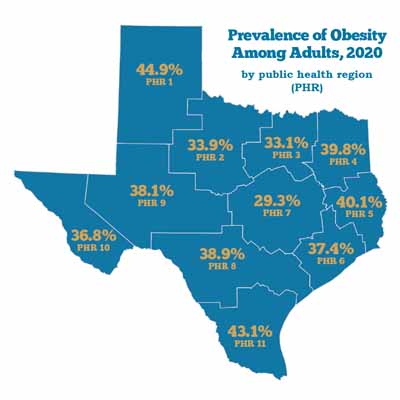
Federal data show a little more than 35% of adult Texans were obese in 2020, placing the Lone Star State just outside the national top 10. State figures are similar. (See “Prevalence of Obesity Among Adults,” below.) These numbers have been increasing for years, and obesity is also relatively elevated among Texas’ youth. (See “By the Numbers: Obesity,” page 37.)
But hope resides outside and inside the exam room.
There is more recognition of the impact nonmedical factors – like food and transportation access, income level, education, and family upbringing – can have on obesity prevalence, and how physician practices can partner with local resources to help blunt the adverse impact of these social drivers of health. (See “Healthy Determination,” September 2021 Texas Medicine, pages 16-23, www.texmed.org/healthydetermination.)
A study released early in 2022 in the Obesity research journal used data from nearly 162,000 adults in the National Health Interview Survey between 2013 and 2017, finding “a graded increase in obesity prevalence with increasing [social determinants of health] burden.”
“Money, transportation, food deserts, all of that plays a role,” Dr. Ramondetta said. “And we spend a lot of time in this country fixing things that are broken, rather than trying to avoid breaking in the first place by putting a bigger emphasis on prevention of disease.”
The Texas Department of State Health Services (DSHS) also has prevention on its radar and through several initiatives is training its sights on the social determinants that correlate with the condition, says Lauren Maxwell, who coordinates DSHS’ obesity prevention programs.
“We know that adults with less than a high school education, low-income adults, adults without health care coverage all experience higher prevalence of obesity,” she told Texas Medicine. “We also know from data that we’ve obtained from our behavioral risk factor and surveillance system that Black and Hispanic adults often experience a higher prevalence of obesity than their white counterparts. As it pertains to Texas geographically, we see a higher prevalence of obesity in areas like the Texas Panhandle and then the Rio Grande Valley as well.”
Knowing obesity is a risk factor for other chronic diseases, DSHS tries to “think upstream,” Ms. Maxwell said, focusing its efforts on systemic support.
For example, some of the state’s obesity-fighting efforts run through the Community and Clinical Health Bridge program, which strives to connect physicians and other practitioners with mechanisms so they can refer patients to community services like food pantries and parks and recreation centers (tma.tips/dshsccps).
There have been challenges in setting up those referral mechanisms, Ms. Maxwell acknowledges. The pandemic made it difficult for health departments and health systems to find staff time to implement those protocols. COVID also introduced several barriers as many of the community and clinical organizations participating had to shift their priorities, “which affected both the level of communication between our partners and the number of referrals during this time,” she said.
The Centers for Disease Control and Prevention and the federal Supplemental Nutritional Assistance Program provide funding assistance to DSHS’ anti-obesity efforts, which also include enhancing:
• Breastfeeding support in the workplace, as evidence indicates breastfeeding an infant is correlated with reduced incidence of obesity later in the child’s life; and
• Food service guidelines in such settings as worksites, community facilities, and early child care and education settings.
Changing the conversation
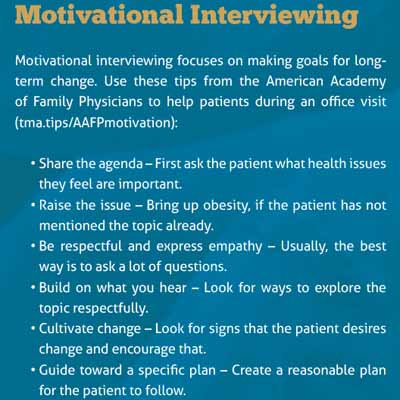
Inside the exam room, Dr. Ramondetta favors concentrated obesity counseling; motivational interviewing; and specific, patient-tailored food-and-exercise prescriptions over blunt, broad-brush admonishments.
Motivational interviewing involves “a lot of listening, not telling,” she said. “It’s about resisting telling somebody what to do and trying to understand their motivations. You’re seeking to understand their values, their needs, to listen with empathy and then to repeat back their own words so that they can see getting healthy is what they really want, too.
“For instance: ‘I hear you say being able to play with your grandchildren is really important to you, and that sometimes you feel like your weight slows you down.’ So repeat back to them their own words so that they can come to the recognition that they want to make this change, and then empower them by providing them with achievable goals.” (See “Motivational Interviewing,” below.)
She adds that managing obesity often requires a multidisciplinary approach, and may involve not only the patient but also family, a health psychology coach or counselor, a nutritionist, or even a physical therapist.
“Tackling obesity and making healthy lifestyle changes is a partnership,” she said.
Some medical schools also are changing the conversation; others don’t quite have expanded obesity programs on their radar. In a 2020 BMC Medical Education survey of 40 medical schools, one-third said they “had no obesity education program in place and no plans to develop one.”
Dell Med, for one, has been working to teach students to refine their approach to addressing obesity with a patient. Dr. Marroquin, the assistant professor of medical education, says a third-year medical student designed the obesity bias module that’s now part of the school’s Developing Outstanding Clinical Skills course.
“She really was concerned that there was a lot of shaming and stigma that patients experienced in the health care system. And oftentimes, they don’t have their care attended to, because people just focus on their weight and just attribute every health problem they have to that,” he said. As a result, “it’s a situation where people don’t ever even want to come back” for additional care.
The module includes students reflecting on their encounters with overweight or obese patients and discussing best practices, such as asking permission to talk about it.
“It’s all about just being kind and respectful,” said Dr. Marroquin, an internist. “Things like … not having the scale in the hallway – having a private area [for weighing]. Asking someone’s permission to weigh them. Asking someone’s permission to talk about weight. Having big enough blood pressure cuffs; things that just make people not feel ashamed, make people feel welcome within health care.”
However, he acknowledges ongoing debate among physicians about how much of an emphasis a patient’s weight should be in the exam room.
“One school of thought is, emphasize good healthy habits, but don’t make a lot of emphasis about losing the weight,” he said, whereas others find it difficult to de-emphasize the link between weight and diseases or conditions such as cancer, diabetes, sleep apnea, and hypertension.
Deborah Conway, MD, vice dean for undergraduate medical education at UT Health San Antonio, believes medical schools should take a broader approach to teaching students how to communicate sensitively to a patient, rather than an obesity-specific approach.
The school does teach about the pathophysiology of obesity and how it’s a risk factor for other conditions, however.
“The place that medical schools need to focus [on] is ensuring that our students are taught, and that our faculty and residents model, treating all patients with dignity regardless of anything,” she said. “Then the skills and the knowledge of how to address overweight and obesity with a patient that meets the patient where they are, a lot of that is going to come in an individual residency program.”
Tex Med. 2022;118(7):34-37
Aug/Sept 2022
Texas Medicine Contents Texas Medicine Main Page