History tells us when gold is involved, word spreads fast.
It happened in California in 1849, despite the efforts of James Wilson Marshall and John Sutter to keep quiet about Marshall’s discovery of gold in the Sacramento Valley the year before. A major event in the history of the American West ensued.
Nearly 180 years later – with word about news of all varieties spreading faster than ever – Texas lawmakers and the House of Medicine have kicked off a gold rush of a different kind.
Oxford, Miss., psychiatrist Katherine Pannel, DO, was sitting in her car waiting to pick up her daughter last year when she browsed social media and found an item on one of the Texas Medical Association’s top legislative priorities of the state’s 2021 session: a way for physicians to shed themselves of insurers’ prior authorization requirements that often stand between patients and necessary care.
Dr. Pannel – chair of the Mississippi State Medical Association’s (MSMA’s) Board of Trustees – says she already was a follower of Texas legislation. In fact, TMA-backed successes at the Capitol become the basis for many MSMA resolutions.
This time, through the double-edged miracle known as Twitter, she learned about House Bill 3459 by Texas Rep. Greg Bonnen, MD (R-Friendswood), which allows physicians to earn a “gold card” out of prior authorizations by demonstrating to insurers that they consistently earn approval for a particular service.
“I went and read [it], I was like, ‘Oh my gosh – Mississippi has got to have this,’” Dr. Pannel said.
With that inspiration, she prompted the writing of an MSMA resolution that directly cited Texas’ gold-card law, asserted the need for “a similar solution,” and resolved for the association to seek a way to streamline prior authorization. The resolution unanimously passed MSMA’s House of Delegates. At this writing, MSMA was preparing to file gold card legislation in the just-begun Mississippi legislative session.
Mississippi is far from the only state that was looking to mirror Texas’ landmark gold card bill, backed wholeheartedly by TMA, which also participated in its crafting. Other states have responded to the development and passage of HB 3459 by contacting TMA in droves, suggesting the measure might not be just a boon for Texas physicians – it could be the start of a major nationwide blow against insurer red tape.
“It makes me really proud of TMA,” said San Antonio radiologist Ezequiel “Zeke” Silva III, MD, who testified for TMA before Texas legislative committees in support of the gold-card bill during 2021. “And it makes me personally and professionally proud to have been someone that was directly involved in this effort. I thought what we did was exactly how the advocacy process from a physician perspective should work.”
Meanwhile, Texas itself is waiting to see how the gold-card law will be implemented. At press time, the Texas Department of Insurance (TDI) hadn’t yet proposed any rules to accompany HB 3459.
Under HB 3459, for state-regulated plans in Texas, physicians can earn a continuous exemption from prior authorization by earning approvals on at least 90% of their preauthorizations on a given service over a six-month period. It also applies to Teacher Retirement System of Texas and Employees Retirement System of Texas plans.
Although that gold card will be continuous after an insurer initially grants it, health plans will have the opportunity to reevaluate physicians’ status up to twice each year. They must notify the physician at least 25 days before a rescission would take effect, with the physician getting a chance to appeal to an independent review organization.
HB 3459 passed with overwhelming approval in its parent chamber and unanimously in the Texas Senate, then became law in June without Gov. Greg Abbott’s signature.
The Harris County Medical Society helped kick-start the push to find a solution to prior authorization headaches several years ago, after it fielded numerous phone calls from members on what was then a nascent problem and engaged TMA and the American Medical Association. Doug Abel, vice president of public affairs and communications for HCMS, says the fruits of that grassroots effort are evidence that physicians can fight back at what’s hindering their practices.
“It’s the importance of letting them know that, hey, you can make a difference. You, the individual physician, can make a difference,” he said. “If you’ve got something that’s hurting your practice, you need to call your county medical society and let them know, and they can take this up to TMA.”
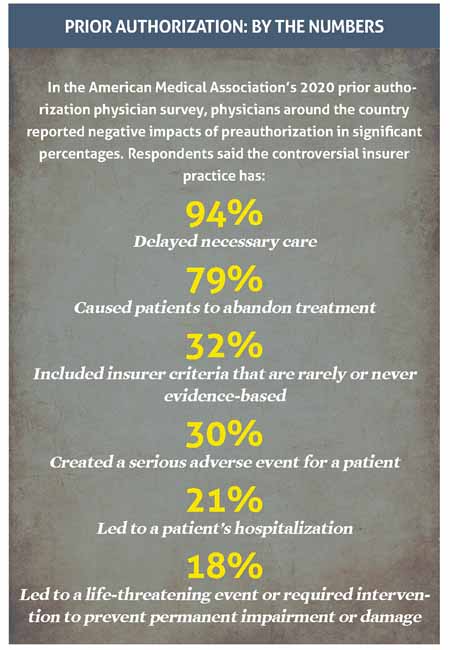
The reason for the new nationwide gold rush is simple: Wherever they are, physicians say prior authorizations are an administrative burden and a care impediment. (See “Prior Authorization: By the Numbers,” this page.)
“Our view in Mississippi reflects the view nationwide: that it’s very cumbersome, time-consuming, and a lot of physicians are having to hire extra staff just to deal with [it],” Dr. Pannel said. “Which in itself is terrible, but the worst part of all is it causes delays in the care by weeks. I’m a psychiatrist. I can’t wait for weeks for my patients to get treatment without [them] committing suicide.
“When it starts affecting patient care that critically, something has to got to be done about it.”
Closer to home, Little Elm internist John Flores, MD – another physician who testified for TMA in favor of HB 3459 – says prior authorizations for his practice’s diabetic treatments are needlessly long in some cases and disrupt the patient’s life.
“The stories are so general because it seems like every single one of my diabetic patients has to play almost diabetes medicine roulette,” he said. “We have to constantly guess what their plans will pay for.”
Sometimes, arriving at that information takes several months for a disease that doesn’t get complacent while the patient awaits a proven, effective treatment.
“I don’t have a specific story, because it’s the same story over and over again,” Dr. Flores said. “It happens so many times, and I’ve got to the point now where I just ask the patients to call their insurance company and ask them, out of the list of medicines I give them, which one they’ll cover. Sometimes multiple times in a year we have to do this.
“It’s frustrating for us, and it’s frustrating for our patients, too. Especially when they’re on a regimen that is working really well.”
As insurers’ preapproval hoops have become more prevalent, medicine’s defenses against them have varied by state. And since word of HB 3459 began spreading, the interest in gold-carding has been swift and broad.
TMA Vice President of Public Affairs Clayton Stewart said “probably over half the states in the country and their medical societies” have contacted TMA with inquiries about how to craft their own version of the bill.
One of the states is Arkansas, where physician advocacy has helped chip away at specific prior authorization problems over the past 10 years, says Scott Smith, director of governmental affairs for the Arkansas Medical Society.
“It’s something that we’ve been living with and dealing with for a long time. And frankly, I think a lot of our members, a lot of physicians in Arkansas, would just as soon blow it up,” Mr. Smith said with a laugh. “Because ultimately, similar to y’all’s situation there as I understand it in Texas, is that most of these get approved. There’s a huge percentage that gets approved, but it’s the delay in care that’s the real frustration.”
He says the Arkansas Medical Society will likely file a gold-card-type bill in January 2023, when the state’s next legislative session begins. He said the bill would “in large part” be patterned after HB 3459.
In Oklahoma, Muskogee general surgeon Jay Gregory, MD, told Texas Medicine he applauds the gold-card law.
Dr. Gregory is a solo practitioner whose staff handles prior authorizations. The main burden for his practice is that prior auth takes time away from other tasks his staff could be doing. And Dr. Gregory confirms the value in a secondary but important piece of HB 3459: It requires peer-to-peer calls occurring prior to a utilization review denial to be conducted by a Texas-licensed physician in the same or similar specialty as the physician who requested the service.
Many physicians who get on the phone with an insurer’s chosen “peer” often find someone speaking the language of a different specialty and a different practice setting. For instance, Dr. Flores recently slogged through a peer-to-peer call for a patient requiring medicine for his diabetic neuropathy.
“Even though this was a generic medicine, they still insisted on a prior authorization and a peer-to-peer. Interestingly enough, the peer that I had to discuss this with was an [emergency department] doctor that had no inkling of the type of practice I run, at least firsthand,” he said. “So that was concerning [to] me.”
Those types of peer-to-peers, he says, are not only frustrating but also can delay care, whereas a similarly specialized clinician can expertly review the treatments a back-pain patient has already had, for example. That clinician can knowledgeably and efficiently determine whether the patient needs magnetic resonance imaging (MRI) to diagnose a pinched nerve.
“If I’m talking to a noninternist that doesn’t deal with back pain, they’re going to say, ‘Oh well, sorry, we’re not going to do an MRI.’ During this delay my patient remains in pain,” Dr. Flores said. “On the other hand, if the peer-to-peer involves a clinician like me, they instead may say, ‘Yes, you’ve done everything appropriate,’ acknowledging that the care delivered was satisfactory.
“It’s faster for everybody and more efficient if they have a colleague in the same field doing the peer-to-peer. Outcomes tend to be better for the patient and for us, and quite frankly for the insurance company, too.”
Dr. Gregory agrees that the relevant knowledge is sometimes only on one end of the phone. Occasionally, when he’s talking to someone of a different specialty, “it’s like talking to a second-year medical student,” he said. “You have to go back and explain the chief complaint, what has been tried, the physical exam, and specifically what we’re looking for on the test that’s being ordered. They don’t have the concept of looking at that from a surgeon’s perspective.”
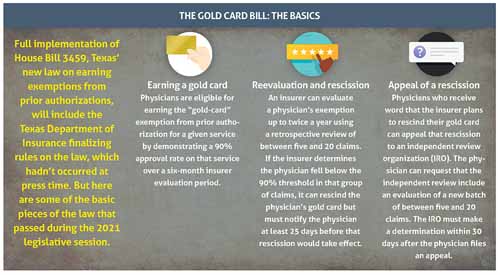
Even as other states prepare their own gold-card bills, Texas’ fight over prior authorization exemptions isn’t over. Officially, the gold-carding provisions of HB 3459 apply to requests for prior authorizations from Jan. 1, 2022, onward. In a practical sense, the Lone Star State was a good distance from true implementation at press time.
The Texas Department of Insurance hadn’t yet released proposed rules for the new law. In summer 2021, TDI requested input from stakeholders. TMA responded with letters that answered TDI’s stated questions about the intent of the law and refuted assertions from insurers about how it should be implemented.
For instance, TMA asserted that while an insurer reevaluation to rescind a gold card requires a retrospective review of between five and 20 claims, the law allows any number of claims – even fewer than five – to be the basis for the 90% approval figure that earns physicians the initial gold card. (See “Texas Prepares to Implement ‘Gold Card’ Prior Auth Bill,” December 2021 Texas Medicine, pages 44-45, www.texmed.org/goldcardprep.)
Still to be determined in rulemaking as of press time was when the six-month review period would begin during which insurers could evaluate physicians’ claims for gold-card status.
However gold-carding ends up looking in practice, Dr. Silva will fondly remember how TMA’s advocacy machine laid the groundwork for the law before and during the 2021 legislative session. And prior authorizations have proved to be an issue both physician and nonphysician lawmakers could relate to.
When Dr. Silva testified for TMA before the Senate Finance Committee last year, “we didn’t have to say anything,” he said. “We were just standing there, and the state senators were telling stories about where they or their families were directly harmed by the prior authorization process. I had five, six stories in my pocket that I could have told; I had to tell one, because they were telling them themselves. And some of them were fairly dramatic.
“We listened to our members, we saw a problem,” Dr. Silva added. “We surveyed physicians to better understand the problem, and once we realized that the problem was even greater than we had predicted from those initial conversations – i.e., some of the patient harm that we saw – we started meeting with legislators. We started gathering our physicians, we started summarizing our issues, and we went into Austin and we built consensus.”
And the result was pure gold.
Tex Med. 2022;118(2):14-19
March 2022 Texas Medicine Contents
Texas Medicine Main Page