
Once dubbed unicorns, value-based care (VBC) models that eschew fee-for-service payment in favor of rewarding quality over quantity have, in fact, materialized.
And a pandemic that has laid bare health disparities has only catalyzed the shift. In fact, “value-based care has spread rapidly across the country, with approximately 40% of Medicare fee-for-service payments, 30% of commercial payments, and 25% of Medicaid payments today being made through some form of value-based arrangement.”
That’s according to a 2021 New England Journal of Medicine article authored by one of the Center for Medicare & Medicaid Innovation’s (CMMI's) own, former director Brad Smith. The Texas Medical Association aims to be on the crest of this wave with the formation of its new Task Force on Alternative Payment Models to help practices navigate the process and resolve thorny issues like too-small incentives, too-great risk, and too many reporting requirements. Here’s a look at some of the major changes in value-based care, and how practices are adapting.
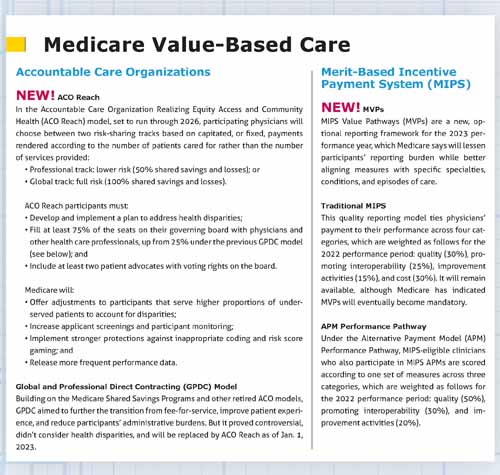
In Medicare value-based care, two major changes will take effect on Jan. 1.
ACO Reach – the Accountable Care Organization Realizing Equity, Access, and Community Health model – will replace an older model and will feature an increased focus on underserved communities and physician leadership. Physicians who are preparing to enroll in this model say it’s a step in the right direction, building on previous iterations while addressing their deficits.
For physicians in specialties and geographic areas without value-based delivery models, the Centers for Medicare & Medicaid Services (CMS) is working to improve upon Medicare’s Merit-Based Incentive Payment System (MIPS) with a new, optional framework – MIPS Value Pathways (MVPs) – it says will reduce physicians’ reporting burden and integrate measures more relevant to their scope of practice. But TMA and others in organized medicine have voiced concerns about building on MIPS’ existing complexity, which only grows more acute with each update.
Meanwhile, commercial payers offer their own value-based contracts as employers and other health plan customers demand better outcomes at lower costs. As a result, Texas physicians are trying to weatherproof their practices for this sea change and soon will have at the ready TMA’s new task force dedicated to value-based care and alternative payment models.
Austin family medicine physician Kevin Spencer, MD – whose practice, Premier Family Physicians, was an early adopter of value-based care – welcomes these developments. As he sees it, physician practices are struggling to maintain already thin profit margins as the American population grows older and as patients shift from commercial plans to public ones, like Medicare, that offer lower and lower payments.
“If you’re dependent on Medicare, Medicare Advantage, and commercial plans, you have to be moving to value,” he said. “It’s not a matter of if. It’s a matter of when.”
Taking VBC to task
As payers and physicians are making the jump to value-based care, so too is TMA. In late April during TMA’s annual conference, TexMed, the board of trustees approved the creation of the TMA Task Force on Alternative Payment Models, whose members will encompass a wide variety of experience with ACOs, bundled payment, capitated payment, Medicaid managed care, Medicare Advantage, MIPS, and more. (See “Calling All TMA Members,” page 24.) Over the next two years, the task force’s roster will leverage its own expertise in value-based care to help other physicians move away from fee-for-service. (See “Value-Based Care for All,” page 20.)
Specifically, its scope of work is to:
- Launch a value-based care survey;
- Identify and prioritize member needs for education, tools, and resources;
- Serve as a touchstone on value-based care policy, advocacy, and regulation;
- Liaise with interested parties and share market intelligence; and
- Develop educational sessions, including an annual value-based care summit.
Value-based care can prove daunting because of its breadth of applications, from public and private payers to every kind of physician practice or employment arrangement, says Kimberly Harmon, TMA’s associate vice president of innovative practice models. It’s also difficult to identify which physicians participate in value-based care because most payers aren’t required to share such information.
Over the next two years and beyond, Ms. Harmon says TMA aims to consolidate its resources and develop new ones – including a physician database – that help members adopt value-based care delivery models without compromising patient experience or their own bottom lines. It will be crucial to hear from those on the ground about what they need from the task force so the effort is physician-driven, she adds.

ACO Reach
Once appointed, the task force could help guide physicians as they transition to new delivery models, like ACO Reach, the latest in a long series of CMS programming intended to facilitate the transition to value-based care.
Since 2010, CMMI has developed more than 50 new delivery models, according to an October 2021 white paper. But only six of those models have generated meaningful Medicare savings. So, late last year, the center launched a strategy refresh, which calls for a more streamlined portfolio of delivery models that “drive health system transformation” and “achieve equitable outcomes,” according to a February 2022 fact sheet.
ACO models are a major component of this new strategy. ACO Reach will soon replace the Global and Professional Direct Contracting (GPDC) model, which no longer aligns with CMS’ pivot, specifically the agency’s new focus on underserved patients. CMS claims this switch will address health disparities, promote physician leadership, and improve patient protections. The transition will affect approximately 26 organizations that involve Texas physicians and health care professionals.
CMS will release more technical information about the model in July, including information about reporting requirements for nonmedical drivers of health. (See “Closing the Loop,” May 2022 Texas Medicine, pages 22-25.)
Meanwhile, Dr. Spencer’s practice is preparing to enroll in ACO Reach. It first joined an ACO in 2014, the early goals of which were to focus on preventive care and offer strategies to better manage patients with chronic conditions, in order to reduce costs associated with preventable emergency department visits and hospitalizations. (See “The Value-Based Care Continuum,” below.)
Under the GPDC model, Premier took the next step to maximize incentive payments by taking on full risk and partnering with a health care technology and management services company that provided value-based care experience and seed money to pay for new clinical programs, care management staff, and other practice infrastructure. This investment led to better patient outcomes and lower costs, driving incentive payments.
Under ACO Reach, Premier will continue to operate in a full-risk model, while assuming new responsibilities to address health inequities. Although this may seem like more work, Dr. Spencer argues it will make the practice more efficient. Premier already operates under a model similar to ACO Reach for its Medicare Advantage patients. Once ACO Reach begins, Premier will be able to standardize its care and data collection processes across its patient population, regardless of their health plan.
“We’re thrilled to get to do that,” he said. “We feel that this is a segment of the population that can get better care, and we’ve got the model to do that.”
MVP or DOA?
For physicians in the earlier stages of the value-based care continuum, CMS will debut a new way for MIPS-eligible physicians to meet their reporting requirements: MIPS Value Pathways. Each pathway includes a subset of measures and activities tied to a specific specialty, clinical condition, or episode of care, according to CMS.
Although MVPs will be optional in the 2023 performance year, CMS indicated in the 2022 physician fee schedule final rule that it plans to make the reporting framework mandatory in the future, starting with multispecialty groups. They will be required to form “subgroups” based on specialty, with each subgroup choosing a pathway to report, in the 2026 performance year.
The seven pathways available starting in the 2023 performance year are:
- Anesthesia;
- Chronic disease management;
- Emergency medicine;
- Heart disease;
- Lower extremity joint repair;
- Rheumatology; and
- Stroke care and prevention.
Here’s how MVPs differ from traditional MIPS:
Under MIPS, a surgeon for instance would choose from the same set of measures as all other clinicians across four performance categories: quality, promoting interoperability, improvement activities, and cost. Under MVPs, however, the surgeon would report only on some measures applicable across the board, such as those related to promoting interoperability and population health. Otherwise, the physician could report on different – and possibly fewer – measures more closely aligned with his or her specialty, such as a quality measure related to surgical site infections.
The “goal is for clinicians to report less burdensome data as MIPS evolves and for CMS to provide more data through administrative claims and enhanced performance feedback that is meaningful to clinicians and patients,” CMS says on its website.
According to the updated scoring hierarchy, even with the new pathway, physicians still will be eligible to receive the highest final score and payment adjustment available from any reporting option – whether traditional MIPS, MVPs, or the Alternative Payment Model (APM) Performance Pathway – and from any participation option – whether as an individual, group, subgroup, or APM entity – except for virtual groups.
Nevertheless, MVPs have prompted some concern from TMA and others in organized medicine, who worry the update will pile on existing administrative burdens within the program.
Jorge Duchicela, MD, a family medicine physician in Weimar and a member of TMA’s Council on Health Care Quality, participates in MIPS. His rural, three-physician practice has had to hire medical assistants to keep up with the program’s onerous reporting requirements. In exchange, he says MIPS offers small incentives, large financial penalties, and little proof it is improving patient outcomes.
“My experience with MIPS has been a love-hate relationship,” he said.
Dr. Duchicela acknowledges the good intentions and hard work that have gone into developing MVPs. But he fears this plan will force physicians like him to adopt a new, unproven iteration of MIPS – or risk financial penalties.
“The specter is that … if you don’t get on board sooner or later, they’re going to ding you for not participating and cut your fees,” he said.
Dr. Duchicela’s concerns about MVPs multiply in the context of the independent ACO he helped create. It spans nine rural practices between Austin, Houston, and Victoria. He already spends a considerable amount of time making sure the other participating physicians are meeting MIPS’ reporting requirements, which is critical to the ACO’s success. But it’s an uphill battle.
“The importance of doing it correctly is huge, but we just don’t have the wherewithal to do it,” he said, adding that the administrative burden associated with MIPS exacerbates physician burnout.
TMA has lobbied CMS to reconsider MVPs and instead focus on the development of voluntary, physician-led APMs, most recently in a September 2021 comment letter. But CMS remains on track to implement the new MVP reporting framework in the 2023 performance year.
The 2023 proposed Medicare physician fee schedule is expected to further address MVPs and their implementation. CMS typically releases the proposed fee schedule in early July.
Tele-value
Still other physician practices are doubling down on value-based care by focusing on telemedicine, sometimes exclusively. Those already in value-based arrangements may find it easier.
During the early months of the pandemic, many primary care practices suffered financially because of government shutdowns and pauses on elective procedures. Although fee-for-service practices had the strongest incentive to resume visits via telemedicine, their value-based care counterparts used telemedicine at higher rates, according to a July 2021 research letter published in JAMA Health Forum.
“This suggests that accountability for cost, quality, and disease management under value-based payment models – and the infrastructure, technology, and management systems of organizations engaging in these models – may have been a stronger catalyst for telemedicine adoption than recouping revenue from deferred in-person visits,” the letter said.
TMA practice management experts say they recently have helped set up new practices that plan to transition to telemedicine-only models in the next few years.
San Antonio emergency medicine physician Randolph Lipscher, MD, plans to open a remote, value-based practice this summer. He anticipates the model will save money on rent and staff by eschewing a brick-and-mortar location while remaining in almost-continuous contact with patients.
But establishing a telemedicine-only practice can be difficult. TMA practice management experts say recruiting patients and employer health plans is even harder without a physical location to attract them. Similarly, such practices may struggle to establish referral and specialist relationships when a patient inevitably needs in-person care, and to get credentialed by payers given the glut of in-person practices already offering telemedicine services.
Telemedicine-only practices also still face legislative red tape unless Congress makes permanent the many telehealth flexibilities adopted during the pandemic, such as the use of audio-only telehealth options; the ability for patients to receive telehealth services anywhere, including at home; and payment parity among both public and private payers.
Dr. Lipscher is hopeful federal and state lawmakers will look more closely at these issues.
“Without the pandemic, we would be stuck in the current paradigm, which is [an in-person], fee-for-service paradigm, for the next 50 years, perhaps,” he said. “That might well bankrupt the country.”
Ogechika Alozie, MD, an infectious disease specialist in El Paso and chair of TMA’s Committee on Health Information Technology, doesn’t believe either modality – telemedicine or in-person – is better suited to maximizing value. But he enthusiastically supports the use of telemedicine to bolster preventive care, improve patient outcomes, and drive down costs.
“Value-based care is value-based care,” he said.
Tex Med. 2022;118(6):12-18
July 2022 Texas Medicine Contents
Texas Medicine Main Page