Did 45 days of social distancing in Texas’ five largest metropolitan areas save more than 40,000 lives and avoid more than 375,000 COVID-19 hospitalizations?
Maybe not exactly, says Laura McKieran, DrPH, the researcher at the San Antonio campus of The University of Texas Health Science Center at Houston (UTHealth) School of Public Health whose work led to an analysis of the impact of “moderate” stay-at-home orders in 30 major U.S. cities.
“No data is ever perfect,” Dr. McKieran said. “I do think it did some good in the most important way, which is that it gave people something positive to focus on and some sense of meaning and purpose to being at home.”
The project began with Dr. McKieran and her team at Community Information Now (CI:Now), a San Antonio nonprofit whose “job is to get data into the hands of people who are working to improve community conditions.” CI:Now is staffed through a community-academic partnership with the School of Public Health, where Dr. McKieran holds an appointment as an associate professor of management, policy, and community health.
“The organization started out the [social distancing] analysis in the negative direction: How many deaths will we have if we do X?” she said. “But we were all already tired of doom and gloom and Armageddon. So we said, ‘Let’s flip it around in the other direction and maybe help people see some value to the incredible sacrifices that we’re making.’”
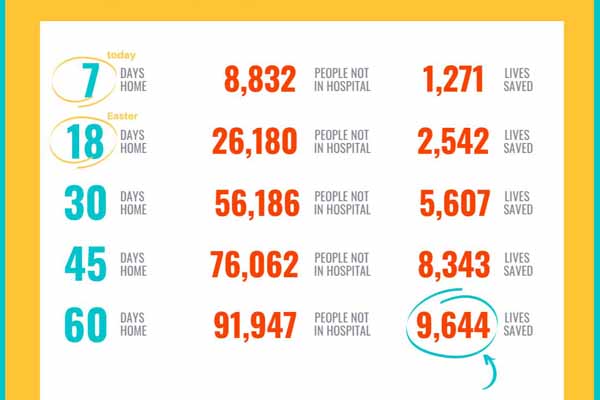
The group started with an epidemiological model published by The New York Times, and calculated estimates for the number of lives saved and hospitalizations avoided in Bexar County over the course of 7, 18, 30, 45, and 60 days of social distancing. They assumed:
- A coronavirus infectiousness measure (or R0) of 2.5;
- A reduction in large gatherings; some school closures; promotion of work from home; and efforts to support hospitals and diagnostic testing;
- A coronavirus incubation period of 5.2 days; infectious period of 2.9 days; recovery time of 11.1 days for mild cases and 28.6 days for severe cases; time to death of 32 days; and a five-day delay before infected patients visit a hospital;
- The average number of infections per-capita in Bexar County would be the same as the U.S. average; and
- South Texas’ warm weather would have a slightly greater mitigating effect than the cooler climates across most of the rest of the country.
CI:Now released its findings for Bexar County on March 31, a week after the San Antonio stay-at-home order took effect. “You saved 1,271 lives last week,” the group announced.
They shared their findings through the National Neighborhood Indicators Partnership.
“This is a super, super, simple method,” Dr. McKieran said.
Partnership members replicated the CI:Now work in Houston, Baltimore, Connecticut, and Philadelphia. There it caught the attention of the Urban Health Collaborative at Drexel University’s Dornsife School of Public Health. That group calculated the numbers for the 30 members of the Big Cities Health Coalition, which announced on May 7 that 45 days of stay-at-home orders in those 30 cities “led to an estimated 2.1 million hospitalizations avoided and over 200,000 lives saved.”
Those are big numbers, especially when compared with the nationwide COVID-19 death count on the Johns Hopkins University & Medicine Coronavirus Resource Center: 104,702 as of June 3; and cumulative hospitalizations (a significant undercount as it tracks only 38 states) from the University of Minnesota COVID-19 Hospitalization Tracking Project: 215,395 as of June 2.
Former Texas epidemiologist Vince Fonseca, MD, who provided technical consultation on the CI:Now analysis, said the project also addressed one of public health’s longstanding problems.
“When public health works, like chlorine in the water, nothing happens. There is no story. ‘Nothing happened today’ is not news,” said Dr. Fonseca, a Texas Medical Association member and associate professor of preventive medicine at the University of the Incarnate Word School of Osteopathic Medicine. “We want to give people some incentive ... we have to make it more tangible to people.”
Dr. McKieran and CI:Now – whose recent data analyses have covered homelessness, autism, racial equity, and voter registration – took satisfaction that their work struck an emotional chord within communities struggling to make sense of an unexpected threat to their health, their lifestyles, and their livelihoods.
“It must have plugged into a spot that people needed to know that there was a reason for this,” she said. “If people saw it and it gave them some sense of hope and meaning to a very tough choice to close, then it served its purpose.”