
Texas physicians who deal with Medicare’s substandard payments and world-class administrative hassles are feeling underappreciated.
The latest report from the committee that advises Congress on Medicare payment policy may exacerbate that feeling.
In March, the Medicare Payment Advisory Committee (MedPAC) released its annual report assessing payments to physicians, among other sectors. MedPAC recommended no changes to the 2021 Medicare physician fee schedule, meaning no increase in physician payments.
Texas physicians see a troubling future for Medicare access if doctors increasingly decide it’s not worth their time to see these patients. That’s why the Texas Medical Association and American Medical Association continuously advocate for fair and adequate payment.
“A lot of these congressional leaders will just assume that we’re going to see [Medicare patients] because we do what’s right and take care of our patients … and we’re going to take care of them no matter what. But at the end of the day, you’ve still got to pay your bills,” said Rio Grande family physician Javier Margo, MD, president of the Texas Academy of Family Physicians. “That’s reality. We’ve already been up against this wall for quite some time, especially in the rural areas.”
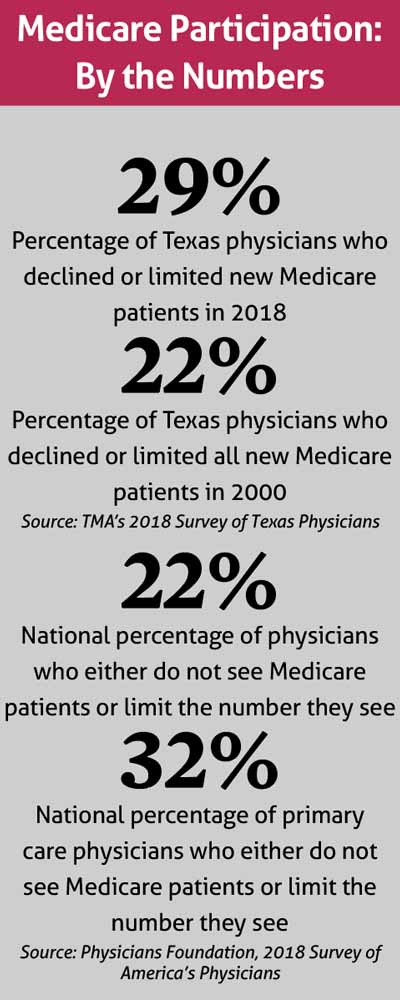
One fifth of Texas physicians were already out of the Medicare game when TMA conducted its last member survey in 2018, an uptick since 2000. (See “Medicare Participation: By the Numbers,” page 36.)
Same money for docs, more for hospitals
The Medicare fee schedule for the next five years already mandates that physicians get no pay raise. However, Congress may adjust the fee schedule for the next calendar year based on recommendations in MedPAC’s annual report.
In explaining its recommendation to hold the line on physician payments in 2021, MedPAC cited access to care for Medicare patients being “largely comparable with” or better than that of privately insured patients; higher satisfaction with quality of care among Medicare patients than among privately insurance patients; and other factors it deemed indicators of “payment adequacy.”
“From 2013 to 2018, the number of clinicians billing the fee schedule grew faster than the number of Medicare beneficiaries, with a slight decrease in the number of primary care physicians more than offset by rapid growth in the number of advanced practice registered nurses and physician assistants,” the report said. “The number of clinician encounters per beneficiary increased modestly.”
MedPAC also said physicians can earn performance-based payment adjustments in Medicare’s Quality Payment Program, a not-so-popular option among physicians since it launched in 2017. (See “An Unfair Game,” January 2020 Texas Medicine, pages 18-25, www.texmed.org/unfairgame.) In fact, MedPAC itself recommended elimination of QPP’s Merit-Based Incentive Payment System in 2018, a recommendation Congress has not acted on.
Meanwhile, hospitals, which routinely receive a small pay increase each year, will get another one in 2021. On top of that, MedPAC’s assessment of Medicare’s performance in acute care hospitals led to an endorsement of a 2% pay bump. If adopted, it would come on top of a 2.8% increase already set in the 2021 fee schedule, which the report notes is the largest for hospitals since 2009. MedPAC said that between 2017 and 2018, Medicare fee-for-service payments for inpatient and outpatient hospital services rose by $6 billion.
“This payment update recommendation is based on indicators of beneficiaries’ access to hospital care, hospitals’ access to capital, hospital quality, and the relationship between Medicare payments and hospital costs,” the report said.
To view the full report, visit tma.tips/medpac2020.
In a written statement, the Centers for Medicare & Medicaid Services (CMS) told Texas Medicine the agency would take MedPAC’s recommendations into consideration for the 2021 fee schedule. CMS also touted changes it made to the 2020 fee schedule to “reduce clinical burden, ensure appropriate payment for clinicians, and enable them to provide their patients with high quality care,” adding that, “this final [2021] rule builds on the Trump Administration’s and CMS’ efforts to secure and improve Medicare and establish a patient-driven healthcare system that focuses on improving health outcomes.”
Pittance + pandemic = trouble
Weimar family physician Jorge Duchicela, MD, estimates half of his practice’s income comes from Medicare. CMS hasn’t “recognized what we bring to the table for their beneficiaries,” he said.
“What happens [with] a rural physician here in Weimar, Texas, for maybe $96.50, you save someone’s life. You save someone’s life! Someone might be having a heart attack, or may have a stroke, or may have a horrible infection, or you’re someone’s grandparent at the nursing home, and [you] have sepsis. That’s what you get paid [to save them],” Dr. Duchicela said. “We do have the best medicine in the world. At least recognize it better than the [compensation for a] barbershop or a hairdresser.”
And at least a hairdresser doesn’t have to deal with additional red tape to get paid, he says.
To make a bad situation worse, the COVID-19 pandemic prompted a serious statewide cutback on nonemergent medical care, Dr. Duchicela adds.
“Our ROI is ‘trying to be alive,’ trying to sustain our practice. I was looking at our collections; they’re down. Most of my practice is almost 98% telemedicine now, whereas we never had telemedicine six weeks ago,” he said. While telemedicine waivers and other temporary CMS rules made such care easier during the pandemic, “it just makes me realize how much better it would be if we would not have all these restrictions that stop me or slow me down from being accessible to my patients, especially in the rural areas.”
In a poll conducted during an April 20 TMA tele-town hall meeting, 60% of physician respondents said their practice revenues were down by half or more since the start of the pandemic. Many physicians across the state also made their first foray into telemedicine during the crisis with 74% of physicians polled saying they began using the technology only after March 1.
Of MedPAC’s recommendation for a 2% hospital pay increase, Dr. Duchicela says the more effective way to drop costs is to incentivize physicians, especially in primary care, which he called a better investment than hospitals, medical equipment, or third-party administrators.
Dr. Margo does his family practice work in a small, nontraditional emergency department. He says Medicare’s fee schedule treats primary care physicians as “basically the bastard stepchild of the medical family tree, so to speak.” That lack of appreciation leads to care deficiencies in rural and impoverished areas, like along the southern border where he practices.
“By and large, you’re going to see a lot of closures,” he said. “I hope it doesn’t happen, but the writing’s on the wall right now. It’s been for some time. If you don’t value primary care the way you should and haven’t been for years, it’s not going to go away. But you’ll have a hard time finding people taking [Medicare] patients.”
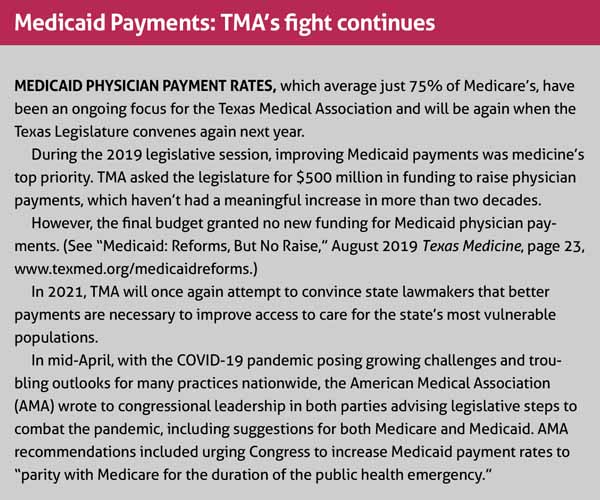
Much of the same dangers exist in Medicaid, where payments are even lower than Medicare and already cause significant access-to-care problems. The lack of adequate compensation in Medicaid is an ongoing priority focus for TMA at the state level. (See “Medicaid Payments: TMA’s Fight Continues,” page 35.)
TMA works for change
Likewise, TMA is doing its part to improve Medicare physician payments. In 2017, the House of Delegates adopted policy urging Congress to “act now to set Medicare fees at an adequate rate and enact requirements for future updates that are adequate to accommodate increasing practice costs.”
In a June 2019 letter, TMA and dozens of other state medical and specialty societies warned congressional leaders that annual updates to the Medicare physician fee schedule “need to reflect increases in practice costs, including compliance with health information technology regulations, quality reporting requirements, and a multitude of other regulatory requirements. ... Therefore, we urge Congress to replace the upcoming physician pay freeze with a stable and sustainable revenue source that allows [physicians] to sustain their practice and provides a margin to invest in the practice improvements needed to transition to more efficient models of care delivery and better serve Medicare patients.”
Keller family physician Gregory Fuller, MD, says he’s noticed a trend among physicians transitioning from traditional Medicare to Medicare Advantage, the Medicare plans administered by commercial insurers.
“In Northeast Tarrant County, we have patients calling up all the time looking for a physician to see a new Medicare patient. In our areas, it’s a problem. There are just not many places seeing new Medicare patients,” he said.
While Dr. Fuller says Medicare Advantage plans have some benefits – such as shared savings for value-based care success – he finds the physician exodus out of traditional Medicare troubling.
“You’re going to have a certain population of patients that for whatever reason, maybe the company they’re retiring from has some kind of Medicare secondary supplement that they provide. It may not be an advantage to go to a Medicare Advantage plan; it may be a disadvantage,” he said. “So then they say, ‘Well, where do I get my Medicare coverage from?’ That might be an issue for patients.”
Administrative roadblocks like prior authorization also make Medicare Advantage options unattractive, Dr. Margo says. Add it all up, and physicians are simply running out of ways to justify taking Medicare.
As for Dr. Duchicela, “older physicians like me, they’re just right at the verge of saying, ‘You know what, I’ve had a good life and I took care of a lot of patients and did my duty, and this is just too much.’ And they just stop,” he said.
Tex Med. 2020;116(6):34-36
June 2020 Texas Medicine Contents
Texas Medicine Main Page