
The delays are done. March 2020 is here, and by law, physicians now must check PMP Aware – the state’s prescription monitoring program (PMP) – before issuing any opioid prescription.
That requirement could’ve caught doctors unaware had it dropped on them during 2019. It was even a possibility back in 2017. But the Texas Medical Association wanted to make sure a required check of the PMP was a doable mandate – one in which technological limitations and roadblocks didn’t make it overly burdensome or outright unrealistic. So, medicine successfully lobbied the Texas Legislature for delays in both years.
Now that integration between PMP Aware and physicians’ electronic health record (EHR) systems is under way, physicians have hope that the mandate – which also requires a PMP check before prescribing or refilling barbiturates, benzodiazepines, or carisoprodol – can do what it was intended to do: crack down on doctor-shopping and drug diversion.
“I’ve seen it help in my own practice,” said state Rep. J.D. Sheffield, DO (R-Gatesville). “Because as a general rule, every patient who’s wanting narcotics gets their PMP pulled, and we’ve had surprises of people who come in with very plausible stories, very believable countenance, but come to find out they’re doctor-shopping and pill-shopping. And without the PMP, we would never have known.”
“They’re always amazed”
When the Texas Legislature gaveled in its 2019 session, the PMP mandate was set to go into effect on Sept. 1 of that year – which itself was the end of a two-year delay granted during the 2017 session. But concerns that the state and its physicians wouldn’t be technologically ready for the transition prompted Representative Sheffield to file House Bill 3284. That measure delayed the mandate another six months, giving time for widespread integration between physicians’ EHR systems and PMP Aware.
“We just felt that the medical profession in general didn’t have the structure in place to do this well,” Representative Sheffield said. “But a pushback to [March 1] would give plenty of time for people to be ready for the implementation.”
During the 2019 session, lawmakers also set aside $5 million for the Texas State Board of Pharmacy (TSBP) to make that electronic integration easier and cover licensing fees for every prescriber and pharmacist in the state.
TMA lobbyist Dan Finch said in January that the integration effort was progressing well.
“The goal has been to roll this out in a predominantly integrated environment in March, not in a predominantly manual environment in September,” Mr. Finch said. “I have to remind doctors [that] the PMP check is required before prescribing opioids, benzodiazepines, barbiturates, and carisoprodol, not all controlled substance prescriptions. But the PMP database should show prescriptions for all controlled substances.
“It’s getting to the point where it is a good clinical database, and doctors will use it as a matter of routine, because it provides them useful information about their patients’ controlled-substance history.”
TSBP Executive Director Allison Benz told Texas Medicine that “quite a few entities” had already undergone the integration and that it speeds up the process.
“This is a tool to help them make a good clinical decision,” Ms. Benz said. “It’s not [that] you see a certain thing [and] you fire your patient.”
TMA’s 2018 Survey of Texas Physicians indicated that 85% of physicians use an EHR. Texas doctors who don’t have an integrated EHR will need to make their required PMP checks by logging into the database at
texas.pmpaware.net.
“There’s always a general frustration with the EHR on the part of physicians,” Representative Sheffield said. “However, talking with some who implemented the PMP into their software to where there’s a simple icon they click on their screen on the patient’s chart, and the PMP pulls up, they’re always amazed how much easier that is to do, and how much information they get almost immediately.”
Be aware
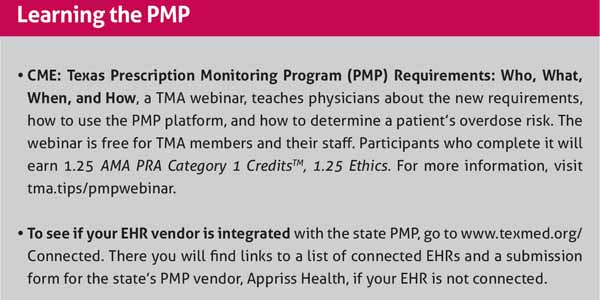
TMA resources are available for doctors who have questions about the PMP requirement and how best to use the database, and whether your EHR is integrated with PMP Aware. (See “Learning the PMP,” above.)
HB 3284 also established a PMP committee to advise TSBP and make recommendations to the board, including recommendations on operational improvements to the database and methods to improve “data accuracy, integrity, and security and to reduce technical difficulties.” The committee, which is chaired by Mesquite pain management physician C.M. Schade, MD, and includes several physicians, met for the first time in January.
“There was absolutely a very positive atmosphere about making this system even better than it is, to smooth out the rough spots, and to look to the future for making this not only easier to use – meaning less keystrokes – but also to make Texas a bellwether state by setting the bar really high on what successful integration looks like,” Dr. Schade said.
The committee’s next meeting is scheduled for April. Dr. Schade says that meeting will include a discussion of how to fund continued integration during the next legislative biennium.
Legal articles in Texas Medicine are intended to help physicians understand the law by providing legal information on selected topics. These articles are published with the understanding that TMA is not engaged in providing legal advice. When dealing with specific legal matters, readers should seek assistance from their attorneys.
Tex Med. 2020;116(3):29-30
March 2020 Texas Medicine Contents
Texas Medicine Main Page