
Institutional racism creates obstacles to medical care. TMA’s Justice, Equity, Diversity, and Inclusion Task Force aims to remove them.
In 2019, Galveston-area endocrinologist Kevin McKinney, MD, faced a situation that remains sadly common for Black men in the U.S.
“I was walking through Home Depot in the town where I live, in League City, and … I passed by somebody’s [shopping] basket and they said, “Hey, what are you doing?’” Dr. McKinney recalled. “She profiled me and thought that I was trying to steal her purse, even though I didn’t notice the purse was there. I was just there doing my own thing. That burned me to no end for a about a day or so. I was so angry.”
Dr. McKinney shared that story at one of the first meetings of the Texas Medical Association’s new Justice, Equity, Diversity, and Inclusion (JEDI) Task Force, which he co-chairs with Pasadena neurologist Kimberly Monday, MD.
During the past two years, the U.S. has experienced a resurgence in awareness of racism. That’s happened in part because people who are Black continue to face “everyday racism,” like the kind Dr. McKinney described. But it’s also happened because of headline-grabbing attacks like the death of Ahmaud Arbery, a young Black man who was shot and killed by white men while jogging in a Georgia neighborhood.
That increased awareness about racism has prompted many corporations and groups like TMA to address what is referred to as institutional racism — biases that are built into the policies, procedures, traditions, and culture of organizations. The TMA Board of Trustees formed the JEDI Task Force to study and report on the impact of racism, inequality, and lack of diversity in medicine while focusing on two primary tasks:
- Examine how these factors affect the public health of patients in Texas and how physicians can mitigate disparities, inequities, and other related concerns; and
- Establish a code of conduct for internal use within the House of Delegates; TMA councils, committees, and task forces; and all other member experiences with TMA.
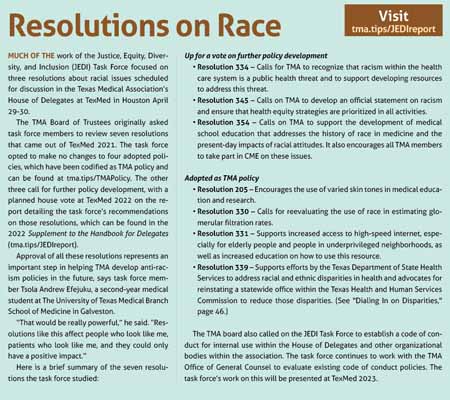
The task force’s findings can be found in its report to the TMA Board of Trustees (tma.tips/JEDIreport). Policy developments on three resolutions were scheduled to go before the House of Delegates at the TexMed 2022 convention April 29-30 in Houston. (See “Resolutions on Race,” page 19.)
“All [of the resolutions] were important in their own way, whether they had to do with the education of physicians or acknowledging that racism is a social determinant of health,” Dr. Monday said. Social determinants of health are the underlying social, economic, political, cultural, and physical conditions people experience where they live and work. (See “Closing the Loop,” page 22.)
The task force’s work began in November 2021, and members quickly found that while TMA has policy against discrimination in general, it lacks specific policy on racism. Many other medical organizations – including the American Medical Association, American Academy of Family Physicians, and American College of Obstetricians and Gynecologists – already have published official statements on racism.
The three resolutions the task force proposed to change are designed to help TMA achieve that goal and help mitigate problems caused by racism in medicine.
“The first thing we did was to recognize that the problem exists,” Dr. McKinney said. “The other thing is that we wanted to be looking forward, not to dwell on the things in the past, but [to see] how can we improve things in the future.”
Early in the process, the 14 task force members discussed their own biases – racial and otherwise – and how those biases affect the way they deal with patients and coworkers, Dr. Monday says. Despite being scientists who are trained to act on evidence, physicians – like anyone – can find tackling personal biases difficult because those biases are hard to recognize. (See “Hidden Brain,” page 28.)
“As a neurologist I find it fascinating to understand the brain circuits responsible for unconscious thoughts that drive implicit bias,” she said. “No one is without bias. If they were, there would be something wrong.”
She added that the task force’s work “is in no way accusatory that any one physician is racist or a bad person. We all have unconscious bias, and if we all understand that, and that it’s not an accusation, then we could move forward, and that would be a win.”
While all physicians should become familiar with their own biases as a first step, the task force’s mission is much bigger in scope, Dr. McKinney says
“This is about [eliminating] the systematic things that have happened in the past [that promoted racism]. Those things are leading to disparate health outcomes right now,” he said “We’re not trying to be divisive. We’re about moving people together.”
Racism and health
Racial and ethnic discrimination have long affected how health care is delivered in the U.S., and they still play a role, according to the task force’s report to the Board of Trustees. “The impact of racism on health has been well documented in research and recognized by organized medicine,” the document says.
For instance, numerous scientific studies have shown over time that patients with darker skin tones of all ages tend to receive lower doses of pain medication than patients with lighter skin tones. More recently, studies have found that people who are Black and Latino suffered disproportionate numbers of hospitalizations and deaths due to COVID-19 compared with white people.
Thanks in part to improved medical care for conditions like cancer and neonatal illness, Black life expectancy has improved in recent years, according to a Sept. 28, 2021, study in the Proceedings of the National Academy of Sciences. In 1990, Black Americans lived seven years less than their white counterparts. By 2018, that number had dropped by more than half, but Black Americans still lived 3.6 years less than white Americans.
In many cases, the disproportionate health outcomes are a result of systemic racism that goes back generations, Dr.
McKinney says. Systemic racism includes practices based on racism that have become ingrained in society over time. In many cases, these practices are no fault of health care organizations directly, but they have a clear impact on people’s health.
For instance, redlining – the now-illegal practice of refusing loans to people who live in certain neighborhoods – kept many Blacks and Latinos living in east Houston. That part of the city remains one of the most heavily industrialized and polluted, creating health problems like asthma.
“Those kinds of things that happened to neighborhoods many years ago tend to have an effect on health outcomes today,” Dr. McKinney said. “You can’t blame that on a specific person. You say that is a systemic problem.”
And social determinants of health often come in groups, says Harlingen psychiatrist Ruthzaine Lopez Bolano, MD, a third-year resident on the task force. For example, one of her teenage Latino patients who needs to take antidepressants comes from a low-income, low-education family and a culture where herbal and home remedies are preferred. Convin-cing the patient to take those medications has been made more difficult by the fact that her family can barely afford the cost of psychiatric care.
“When you think about all the components of health – not just the biological component, but the social, economic, and political – it is really complex to address all that if we don’t have policies in place to mitigate that and facilitate the access to health care,” Dr. Bolano said. “I am hopeful by getting smart people together and creating policies, perhaps in five or 10 years, health care access to vulnerable populations will be more affordable and fair.”
Physicians have a long history of stereotyping patients, particularly low-income ones, Dr. McKinney says.
For instance, patients who fail to follow the course of treatment laid out by a physician may be dismissed with the term “noncompliant” and sometimes dropped from a practice. Dr. McKinney believed that one of his patients with diabetes was especially noncompliant – ignoring all treatment advice after three or four visits. But then he found out that she had family problems that kept her from following his treatment.
“After those issues were resolved, she started taking care of herself a little bit better,” he said. “You should always look for the deeper meaning. Most patients are not intentionally noncompliant. I think that’s one area where we fall short with stereotyping.”
Systemic solutions
Much of the task force’s time so far has focused on the three resolutions scheduled to be discussed by the House of Delegates at TexMed. Once that is complete, the group will keep meeting throughout 2022 and into 2023 to address other diversity issues in Texas medicine.
“They’ve always been there, they just haven’t been addressed,” said task force member Tsola Andrew Efejuku, a second-year medical student at The University of Texas Medical Branch School of Medicine in Galveston. “A big organization like TMA addressing them is important – using its power to make things more equitable not only for patients but for physicians as well.”
For example, research shows one impactful way to improve health outcomes for patients of color is to increase the number of physicians of color, many of whom are underrepresented in medicine. (See “Preparing the Path,” page 33.)
Texas medical schools are working to boost those numbers among graduates, Mr. Efejuku says.
“I’ve seen a lack of diversity, but I’ve also seen efforts being made on the institutional level at my school and also, hopefully, at the state level to increase that diversity to make the process more equitable so that you get all kinds of physicians to treat all kinds of patients.”
One of the pending resolutions, if approved, would call on TMA to work with medical schools to better understand their current curricula with regard to diversity and equity, and encourage the development of education that addresses the history of race in medicine and its present-day effects on historically marginalized ethnic groups.
“We’re not asking for curricular mandates,” Dr. McKinney explained. “We’re surveying what medical schools are doing already so we can help amplify or publicize those things [they have] done well.”
That education doesn’t stop with medical schools. The resolution also encourages all TMA members to take part in CME on these issues. And physicians who want to know more about the JEDI Task Force’s work can read its report and contact task force members with questions, Dr. McKinney says.
“We want to each be available to those who have questions about [the report],” Dr. McKinney said. “Some people feel that just bringing up the issue of race is divisive. But if you understand that these are things that have been around for a long time that we’re trying to eliminate, and that we’re not trying to pigeonhole any one person [on the subject of race], you’ll see we’re going after systemic problems. Systemic problems need systemic solutions.”
The task force’s work also is designed to help physicians do their jobs better by clarifying issues tied to justice, equity, diversity, and inclusion, Dr. Monday says.
“If we have everybody thinking of this … when they’re dealing with patients, then that will be a success,” she said.
Tex Med. 2022;118(5):16-21
May 2022 Texas Medicine Contents
Texas Medicine Main Page