Prior authorization of health care services has become a burden and a barrier to physicians providing the care their patients need.
Health plans maintain they require prior authorizations to ensure requested services are medically necessary and appropriate. But the escalation of prior authorization use may also be motivated by a desire to control costs.
A 2020 survey of Texas physicians revealed they have seen a drastic increase over the past five years in the burden of prior authorization on their patients and their practices. In fact, 87% say this burden has increased and nearly half (48%) of physicians have had to hire staff solely to process prior authorization requests. [1]
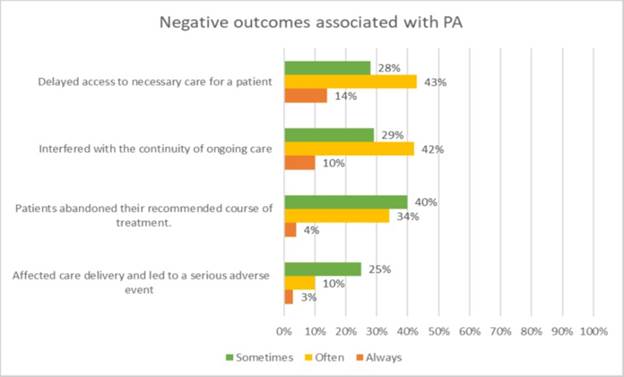
Prior authorization was meant to be a check on the medical necessity of expensive and less common services and treatments; however, insurers increasingly apply it to basic and routine patient care, which needlessly may delay much-needed services. Surveyed Texas physicians also reported having to obtain prior authorization for medical procedures (80%) and prescription medications (85%), even common and generic ones. They reported completing on average 31 prior authorization requests a week, taking time away from patient care. Four-fifths (85%) reported prior authorizations delayed patient care, and 78% said this can lead patients to abandon needed treatment altogether. Thirty-eight percent indicate it has led to an adverse event for their patient
TMA asks for support of legislation that removes these barriers to patient care and allows physician practices to spend more time with patients – and less time on the phone with big insurance companies.
TMA's Legislative Recommendations
- “Encourage review of medical services and prescription drugs requiring prior authorization on at least an annual basis, with the input of contracted health care providers and/or provider organizations.” [2]
- “Support continuity of care for medical services and prescription medications for patients on appropriate, chronic, stable therapy through minimizing repetitive prior authorization requirements.” [3]
- Require health benefit plan issuers to “gold card” certain physicians from prior authorization (i.e., create an automatic approval or exemption, on a physician-by-physician basis, that waives prior authorization requirements if that physician is approved for a specific procedure/service the vast majority – e.g., 80% – of the time).
- Require the Texas Department of Insurance to audit health plan compliance with statutory prior authorization timelines for approvals and denials.
- Strengthen Texas law to better prevent payment denials once patient care has been approved.
- Prohibit prior authorization for health care services that are state-mandated benefits: mammography, mastectomy and breast reconstruction or prosthesis, diabetes management, low bone-mass test for osteoporosis prevention, and prostate cancer screenings. As health benefit plan issuers are required to cover these, prior authorization is an unnecessary barrier to patient care and a misuse of physician time better dedicated to patient care.
- Heighten enforcement and penalties when a health benefit plan issuer or its agent (1) knowingly violates the prudent layperson standard for emergency care; (2) deters enrollees from seeking care consistent with the prudent layperson standard for emergency care; or (3) engages in a pattern of wrongful denials of claims for emergency care, including denials related to application of the prudent layperson standard.
- Require peer-to-peer discussions under Tex. Ins. Code §4201.206 (b) to be with a Texas-licensed physician who is of the same or similar specialty. For example, for a cancer treatment ordered by an oncologist, a Texas-licensed oncologist should conduct the peer-to-peer call on behalf of the utilization review agent, not a physician in an unrelated specialty.
- Require health benefit plan issuers and benefit managers that require prior authorizations to have staff available to process approvals 24 hours a day, 365 days a year, including holidays and weekends. [4]
[1] Preliminary results from February 2020 survey by the Texas Medical Association; final report pending.
[2] Consensus Statement on Improving the Prior Authorization Process by the American Hospital Association, America’s Health Insurance Plans, American Pharmacists Association, Blue Cross Blue Shield Association, American Medical Association, and Medical Group Management Association.
[3] Id.
[4] The American Medical Association recently adopted policy to this effect.
Texas Legislature main page
Last Updated On
February 05, 2021
Originally Published On
January 20, 2021