Sometimes it sounds like nothing but noise.
During a national election year, candidates rip each other. Campaign “surrogates” do the same. Candidates may have approved that message, as the ads typically say, but you didn’t approve receiving it. Meanwhile, mailers and fliers abound.
While all that’s going on, Texas physicians just keep trying to do what’s best for their patients – sometimes running into reminders of how the system needs to do better by those patients.
One year from now, Texas voters will hit the polls. They’ll be voting for president, for Congress, and for seats in the Texas Legislature. At the state and national levels, health coverage, Medicaid access, and prescription drug costs have gotten plenty of attention already, and they’ll get plenty more between now and the closing of the polls on Nov. 3, 2020.
Here’s a look at some of the major health care debates taking center stage during the 2020 election cycle, what voters are and will be hearing about, and what Texas Medical Association policy says on those particular issues.
Health coverage
Nearly a decade after passage of the Affordable Care Act (ACA), health care coverage remains front and center in the presidential race.
Not long ago, single-payer proposals – or proposals billed as such – were a bridge too far for any major presidential candidate. But this cycle, several leading Democratic candidates are pushing for a dramatic overhaul of the nation’s health insurance law.
TMA policy is clear: Single-payer systems “are not in the best interest of the public, physicians, or the health care of the nation.” (Check out all official TMA policy positions at www.texmed.org/Policy.) Debates and worries over costs and logistics of such plans rage on, and they’re not going away anytime soon. But the notion was inescapably in the conversation this summer.
Sen. Bernie Sanders (D-Vt.) champions such a government-run, single-payer proposal, and introduced a Medicare-for-all measure this year. Sen. Kamala Harris (D-Calif.) has a plan billed as Medicare for all, but it would allow private insurance to offer Medicare plans and includes a 10-year transition period to the new system. One of Texas’ two candidates for the Democratic nomination, former U.S. Rep. Beto O’Rourke (D-El Paso) is offering an alternative he calls “Medicare for America” that would give people whose jobs offer private insurance the option of taking either their employer’s plan or Medicare.
Former Vice President Joe Biden, however, is running on protecting and building on the ACA. His plan includes adding a “public option” to the ACA system that would compete with private insurers, and offering premium-free access to the public option for adults who would’ve been eligible for Medicaid if their states hadn’t refused the ACA’s Medicaid expansion. (Texas is one of those 14 states.)
Despite all the competing rhetoric, San Antonio neonatologist Alexander Kenton, MD, says health insurance coverage is probably the “least thought-out of all topics” in the campaign. Dr. Kenton is a former chair of TEXPAC, TMA’s nonpartisan political arm that endorses and raises money for medicine-friendly candidates. He notes the ACA framework was years in the making before its passage in 2010; likewise, he says, it will take four to eight years of planning to come up with a comprehensive proposal to significantly overhaul health care delivery in the U.S.
“The only thing people know is they’re not happy with the current way health care is delivered in this country. That’s the only thing people actually know,” he said. “And it’s because insurance prices are too high. The monthly fees, or what’s taken out of the paycheck … are too high. The deductibles are too high, and the coverage is too little.
“But the problem is that all these folks that are standing up and putting out the proposals, they haven’t worked behind the scenes to actually come up with a comprehensive strategy.”
For instance, if a public-option “safety net” becomes part of the ACA, Dr. Kenton asks, “Are you going to provide end-of-life care to everybody who’s terminal and irreversible, or are you going to make a decision that you’re not going to cover those things?” Similar decisions would have to be made for procedures and conditions like dermatology interventions, knee replacements, and sexual disorders, Dr. Kenton adds.
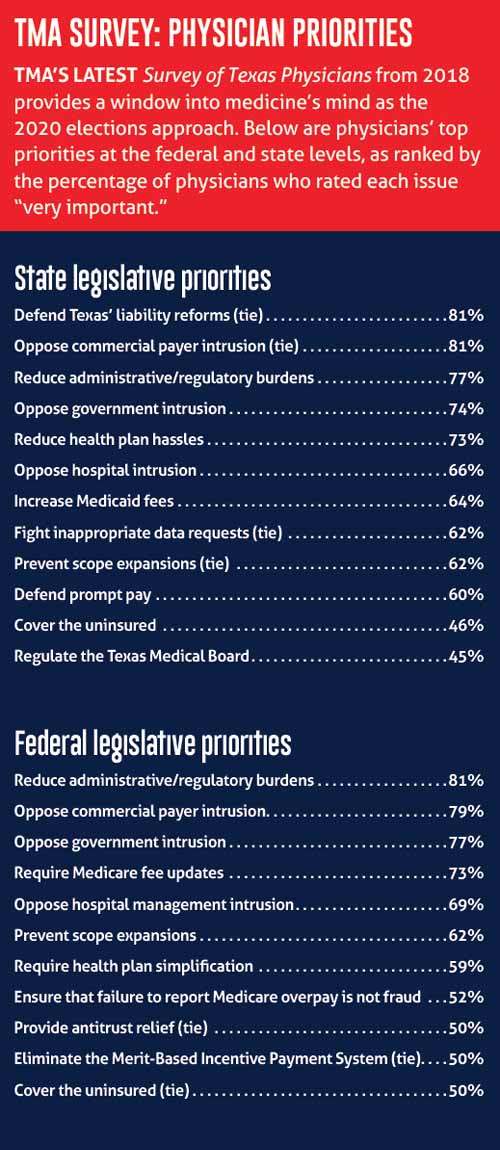
Although TMA’s every-other-year Survey of Texas Physicians shows the majority of Texas physicians don’t support a single-payer system, support for it increased significantly in TMA’s latest survey in 2018. The percentage of respondents who said they support single-payer rose from 36% in the 2016 survey to 46% in 2018. (See “TMA Survey: Physician Priorities," page 21.)
The Trump administration had not released a health care plan as of press time in late September, although the Wall Street Journal reported in August that the president was considering rolling one out in October. President Donald Trump’s campaign website touts health care “achievements” during his first term, including removal of the ACA’s individual mandate to purchase insurance coverage.
Medicaid
Unfinished business on Medicaid coverage and access to care for low-income and uninsured Texans will be on the minds of members of TMA’s Select Committee on Medicaid, CHIP, and the Uninsured, says committee chair Maria Scranton, MD.
The Round Rock pediatrician knows firsthand these programs’ shortcomings. She’s treating a 4-year-old patient whose family, because of a slight increase in income, no longer qualifies for the Children’s Health Insurance Program (CHIP). The child now has coverage through one of the ACA’s exchange plans. But having to pay for that coverage out of pocket leaves the family’s take-home pay less than it was when the child had CHIP coverage, Dr. Scranton says.
“You can see how people get in these cycles where if we could address these [health care] issues in a beneficial way, … our working people could be able to move ahead in life. I think that needs to be a focus.”
TMA policy supports drawing down all available federal dollars to expand access to health care for poor Texans while implementing a Texas-designed, Texas-specific Medicaid program. TMA policy also says CHIP eligibility should be offered to the highest extent allowed by federal law.
The committee still aims to extend postpartum Medicaid coverage to 12 months as well, something TMA unsuccessfully pushed for during this year’s Texas legislative session. Dr. Scranton also wants legislators to address Texas’ high rate of uninsured patients and to increase physician payment rates in Medicaid, which have gone decades without a meaningful increase. This year, TMA asked the legislature for a significant Medicaid payment bump, but state lawmakers didn’t grant it.
“That is still going to be extremely necessary,” Dr. Scranton said. “Once these people get coverage, they need to have access to care. But if the rates don’t go up, it’s very, very difficult to continue to have a pool of places that they can go and access coverage. We can’t let that fall by the wayside.”
Among other tenets, TMA policies on Medicaid and CHIP call for the association to advocate for Medicaid managed care reform, to oppose Medicaid and CHIP funding cuts, and to work for physician payment parity in Medicaid and CHIP.
Surprise medical bills
At the federal level – where the vast majority of health insurance plans are regulated – the debate over how to address surprise billing heated up this summer. The 2019 Texas Legislature took a big step in addressing surprise medical bills for state-regulated insurance plans. But state-regulated plans account for less than 20% of the plans on the market.
Dr. Kenton calls the surprise-billing debate “the single most pressing issue for physicians to practice the way they have in the past.” He says without a fair solution, there’s a significant risk that “almost no physician will be independently practicing anymore – that they will all end up being employed, because they won’t be able to survive as a small business.”
As such, organized medicine was feverishly trying to steer the congressional conversation on balance billing in physicians’ favor, while simultaneously working to take patients out of the middle of out-of-network billing disputes.
Specifically, medicine was encouraging Congress to embrace independent dispute resolution (IDR) inspired by the successful system enacted in New York – which influenced Texas’ overhaul in this year’s Senate Bill 1264. The measure features a “baseball-style” arbitration process for out-of-network billing disputes on state-regulated plans. TMA’s advocacy made sure SB 1264 gave physicians a fair shake in determining their payment by including billed charges in the factors that determine the final payment. (See “Swinging for Fairness,” August 2019 Texas Medicine, pages 30-31, www.texmed.org/swingingforfairness.)
During the summer, TMA and the American Medical Association (AMA) warned Congress about the unfairness of government-established benchmarking for out-of-network bills. They cautioned that a government-benchmarking scheme has failed in California, where a 2016 law dictated physicians be paid either a “median in-network rate” determined by the health plan or 125% of Medicare. That law has led to insurers dropping physicians from their networks and refusing to contract with them.
At press time, federal measure H.R. 3630, known as the No Surprises Act, included a compromise between government-benchmarking and arbitration. It would allow either the health plan or the physician to appeal to an arbitrator in disputes where billed charges exceed $1,250.
TMA policy supports the AMA’s stance on balance billing for Medicare recipients. AMA states that physicians should be allowed to balance-bill for the difference between Medicare payments and physician charges.
Debra Patt, MD, chair of TMA’s Council on Legislation, calls the surprise-billing debate “a tough balance, like all things in medicine.
“It’s important to protect patients from surprise bills, but yet, it’s hard to ban surprise billing and still allow payers to negotiate in reasonable ways with doctors,” she said.
Prescription drugs
A frequent target of President Trump’s tweets, prescription drug prices seemingly please no one except, perhaps, drugmakers. While analyses vary on how much prescription prices are going up, the widespread consensus is that they’re still rising.
In a July analysis, Rx Savings Solutions, an online medication price look-up tool, found that the prices of more than 3,400 drugs had risen so far in 2019. Prices for those drugs rose by an average of 10.5%, or approximately five times the rate of inflation, the study found. The topic has come up repeatedly on the campaign trail, and it’s not likely to slow down as the election approaches.
TMA Vice President for Advocacy Darren Whitehurst says pharmaceutical companies often provide no justification for exorbitant price increases.
“I do think at the very minimum, transparency and some of these arrangements between the PBMs (pharmacy benefit managers) and the insurance companies and the pharmaceuticals … shedding light on some of those practices would probably alleviate some of the things that are going on in the marketplace today,” he said.
Former Vice President Biden’s plan to tackle prescription drugs includes a repeal of the law that prohibits Medicare from negotiating prices with drug manufacturers. He also calls for the creation of an independent review board that would limit the prices for new specialty drugs that face no competition. The board would assess the value of the drug and recommend a reasonable price, which would be what Medicare and the public option would pay for the drug.
Senator Sanders’ plan also calls for allowing Medicare to negotiate with the major drug companies. And both he and Mr. Biden would allow patients to buy prescription drugs from other countries.
In May 2018, the Trump administration released a plan to reduce prescription drug costs that centered on improving competition, improving government negotiation, incentivizing lower list prices, and lowering out-of-pocket costs. Planks of the plan included exploring a requirement to list drug prices in advertising and banning “pharmacy gag clauses” in Medicare Part D contracts, which prohibit pharmacists from telling patients when they could pay less out of pocket by not using their insurance.
However, in July 2019, the Trump administration backed away from a key proposal to help fulfill its plan: a rule that effectively would have prohibited drug manufacturers from giving certain rebates to health plans and PBMs for Medicare Part D and Medicaid plans. The administration cited the prospect of increased premiums as the reason for withdrawing the rule. The same month, a federal judge blocked the administration’s proposed rule to require drugmakers to reveal the price of certain drugs in TV ads. Also in July, the administration announced it would create a system to import lower-cost prescription drugs from Canada.
TMA policy says the association will support programs to contain rising prescription-drug costs as long as the program satisfies several criteria. Among them:
• Physicians have significant input in developing and maintaining the programs;
• All patients must have access to medically indicated prescription drugs necessary to treat their illnesses; and
• Physicians must have the freedom to prescribe the most appropriate drugs and method of delivery for individual patients.
Opioids
Opioid addiction and overdoses have dominated headlines the past several years, as well as election debates. Opioids have been extraordinarily costly both in lives and dollars. A 2016 study by the National Center for Injury Prevention and Control estimated the cost of prescription opioid overdose, abuse, and dependence to be $78.5 billion during calendar year 2013, with increasing health care and substance abuse treatment costs accounting for more than one-third of that.
An early rhetorical focus of the Trump administration, the crisis led to the president declaring a national emergency in 2017, a year in which opioids accounted for 68% of all drug overdose deaths, according to the Centers for Disease Control and Prevention. The U.S. Department of Health and Human Services (HHS) says between the beginning of the Trump administration and the end of 2019, the agency will have awarded more than $9 billion in state and local grants to help increase access to treatment and prevention services. The Substance Abuse and Mental Health Services Administration has granted more than $116 million in funding to Texas over the first two years of the State Opioid Response program in 2018 and 2019, according to HHS.
Democratic candidates also want to use the full force of the federal government to tackle opioids. The CARE Act of 2019, introduced by Sen. Elizabeth Warren (D-Mass.) in May and cosponsored by Senator Sanders, would provide $100 billion over 10 years to fight the crisis. According to a column written by Senator Warren on the website Medium, the measure includes $4 billion annually for states, territories, and tribal governments, and $500 billion per year to expand access to the rescue drug naloxone.
TMA policy supports “multidimensional strategies to optimize the treatment of pain.” That aspect often gets lost in the discussion, says Houston pain management specialist Brian Bruel, MD, president of the Texas Pain Society. While Dr. Bruel agrees with devoting both dollars and attention to addiction treatment, he says there’s another key piece of addressing the epidemic: Using other available methods to treat pain and its ripple effects.
“The Pain Society and other societies have all talked about the different modalities, including psychologic treatment, including interventions, including non-opiate pain medications that might be effective for these patients long term. The problem is, that’s not really talked about as much as we would like,” he said. “A lot of the focus, because of the opiate crisis, has been on the pharmaceutical industries, has been on the costs of opiates, has been trying to place blame [for] the crisis. I think there’s not just one person or society or group to blame. It really, truly is multi-faceted.”
Texas could receive crucial dollars to fight the opioid epidemic at the state level now that drug-maker Purdue Pharma has agreed to settle a lawsuit filed by Texas and more than 20 other states. (See “Easing the Pain,” page 24.)
Tex Med. 2019;115(11):18-23
November 2019 Texas Medicine Contents
Texas Medicine Main Page