
High participation, “significant strides,” overwhelming success.
That was the picture the Centers for Medicare & Medicaid Services (CMS) painted in a March report on the first year of the Quality Payment Program (QPP). The overall participation rate in the program’s Merit-Based Incentive Payment System (MIPS) during 2017 was “exciting,” the CMS report said. MIPS participation among rural practices was “a remarkable accomplishment,” according to the agency. And the number of small and rural practices that submitted more than the required minimum of data showed those clinicians were “committed to meaningfully participating in MIPS to continue driving value and innovating to improve patient outcomes.”
But a closer look by the Texas Medical Association raises serious doubts about CMS’ numbers, transparency, and cheerleading – so much so that TMA and seven other state medical associations are asking the agency to rescind the report.
In April, after carefully analyzing CMS’ 2017 Quality Payment Program Reporting Experience report, TMA spearheaded a joint letter from eight of the 10 members of the Coalition of State Medical Societies. The letter urges CMS to rescind the report and “establish a transparent approach to your analysis and reporting, and issue a revised, unbiased, and complete report that truly captures the full breadth” of the QPP’s first year.
In reaching that recommendation, the letter lays out a detailed case for what’s missing – and why the report poses a danger if it’s accepted as a definitive portrayal of the QPP’s first year. (CMS assesses MIPS payment adjustments two years later, and 2017 results affect physicians’ Medicare payments in 2019.)
“Given the magnitude of this program and the goals it sets out to achieve for the Medicare patient population, physicians deserve a report that is truly comprehensive in nature, covering every aspect of the QPP experience, including whether the program is resulting in improvements in care quality, efficiency, patient safety, and overall population health outcomes among our Medicare beneficiaries,” the letter says.
Furthermore, medicine expressed deep concern about the negative impact the program truly may be having on small and rural practices in particular: “Overall,” the letter says, “it is our impression that the data has been distorted to minimize the reality of the adverse impact the QPP has on small and rural practices, as well as on physician practices at large.”
The report “lacks detail. It doesn’t allow us to drill down,” Austin colon and rectal surgeon David C. Fleeger, MD, TMA’s newest president, told Texas Medicine. “It counts physicians who were exempted because of Hurricane Harvey in the state of Texas as participating.
“It was a year that was very easy to participate in, and each year is going to become more onerous. And yet we still have a significant number of physicians that aren’t [participating], and I suspect that number will probably actually increase as the requirements become more onerous.”
Questionable and misleading data
Joining TMA on the letter were the medical societies from California, Florida, Louisiana, New York, North Carolina, Oklahoma, and South Carolina. It was addressed to both U.S. Department of Health and Human Services Secretary Alex Azar and CMS Administrator Seema Verma.
The medical societies cast doubt on CMS’ claim of a 95% overall participation rate in QPP, noting that its appendix shows a 97% participation rate in Texas – even though the Hurricane Harvey exemption covered every clinician in 53 Texas counties. Those exempt clinicians automatically received a MIPS final score of three points that kept their “payment adjustment” neutral; in other words, no penalty or bonus.
According to the report’s statistics, just under 61,000 eligible Texas clinicians participated; 1,830 did not.
Per medicine’s analysis, however, it appears the agency counted both clinicians who submitted data and those who were exempt, which may have artificially inflated the participation rate and created “an illusion of exceeding expectations” in year one.
“Because CMS was not transparent in providing the number of clinicians who received an automatic three points under this policy, and without an accurate accounting of true participation through meaningful submission of data, these participation rates may not be accurate,” the letter states. “We would like to know how many physicians in our states and nationwide truly submitted data in the 2017 QPP.”
CMS also leaves out the percentage of clinicians who met the QPP’s data requirements across all three of the weighted MIPS categories for 2017: Quality, Advancing Care Information, and Improvement Activities.
“This rate would be the true measure of success for program participation,” medicine’s letter states. “Other than general participation counts and other incomplete data pertaining to data submission, it appears CMS cherry-picked the data that would make the QPP look favorable and left unreported data that would expose some of the major shortcomings of this program.”
Because of the incomplete information, TMA was “unable to conduct a comparative analysis among all reporting levels,” such as individual practices versus groups, small practices versus large, and to analyze how certain specialties did, among other data slices.
And buried in the report’s appendix is information showing that more than 15,000 clinicians in the eight states combined didn’t participate during year one.
That so many clinicians “would prefer to sit out of the QPP in 2017 and suffer a 4% payment penalty this year rather than hassle with participation is significant to us and bad for medicine,” the state medical societies wrote.
Harm to small and rural practices
The QPP is a budget-neutral program, meaning the bonuses and penalties that result from it have to even out. And the CMS numbers show that small practices – defined in the QPP as those with 15 clinicians or fewer – are footing the bill for larger-shop participants better equipped to handle QPP’s practical and technological rigors.
According to CMS figures, more than 51,000 clinicians nationally fell short of the program’s benchmarks in 2017, meaning those practices incur a 4% Medicare payment penalty this year. Of those 51,000-plus, 83% are clinicians from small practices, and 18% are from rural practices.
“We can conclude that, due to budget neutrality, 2019 MIPS incentive payments are funded mostly off the backs of clinicians in small and rural practices nationwide. Moreover, almost one-third of the clinicians who are actively receiving the 4% payment penalty this year are from our states and are funding the 2019 MIPS incentive payments for the rest of the country. This does not illustrate a successful first year as CMS reports, and it is wholly unacceptable to us.”
TMA and the other societies also take CMS to task for not including any data for their states that compares the performances of large practices to small and rural ones, as well as for not showing how physicians in those states did relative to the rest of the country.
“We need this data to assess the FULL experience in the QPP and the move to value-based care in general, as well as to identify opportunities for education and technical assistance and to inform our ongoing advocacy,” the medical societies wrote.
Keller family physician Greg Fuller, MD, a member of TMA’s Council on Socioeconomics and that council’s liaison to the Council on Health Care Quality, saw the CMS report as a generic document that doesn’t address whether QPP improves patient care and outcomes.
“We don’t want to penalize the most vulnerable physicians – rural and small groups – who probably are doing a lot of Medicare and Medicaid anyway,” he said. “My other thought was, how much work did [physicians] do to get their miniscule raise? That’s always been my concern, is just the high cost of trying to do these things.”
The highest available 2019 bonus, awarded to clinicians who met the target for “exceptional performance” in 2017, was just 1.88% of their Medicare claims. For everyone who earned a bonus but didn’t meet the “exceptional” threshold, the top possible bonus was 0.20%. CMS reported that “remarkably,” 93% of eligible clinicians earned a bonus payment in 2017; 2% received neither a bonus nor a penalty; and 5% received a penalty.
Recommendations
The first year of the QPP also featured elements that made it relatively easy to participate and achieve success in the program, or to be exempt from it, medicine’s letter notes. Those included:
- The exemption for Harvey-affected physicians and others affected by 2017’s numerous hurricanes and the California wildfire;
- The low-volume threshold that exempted many physicians (still maintained in the current version of the program);
- The “pick your pace” option that allowed clinicians to select a bare-minimum level of reporting;
- A lower performance target (just three points to avoid a penalty, which increased to 15 points in 2018 and 30 in 2019); and
- The fact that the MIPS Cost category wasn’t a weighted factor in 2017.
“Because some of these mitigating factors no longer exist, we foresee future outcomes in our states in which potentially thousands more receive the payment penalty,” medicine’s letter says. “We believe there is an urgent need for CMS to prioritize QPP improvements to ensure broad physician participation.”
TMA and the other societies fear the report’s “inaccurate narrative” may be “used erroneously” to validate a decision to modify the low-volume threshold for exemption. Reducing or eliminating the low-volume threshold would deliver “disastrous consequences for small and rural practices,” the letter says. While CMS claimed the report was based on “feedback … from clinicians, stakeholders, researchers, and others,” the eight societies say CMS didn’t seek input from any professional medical associations.
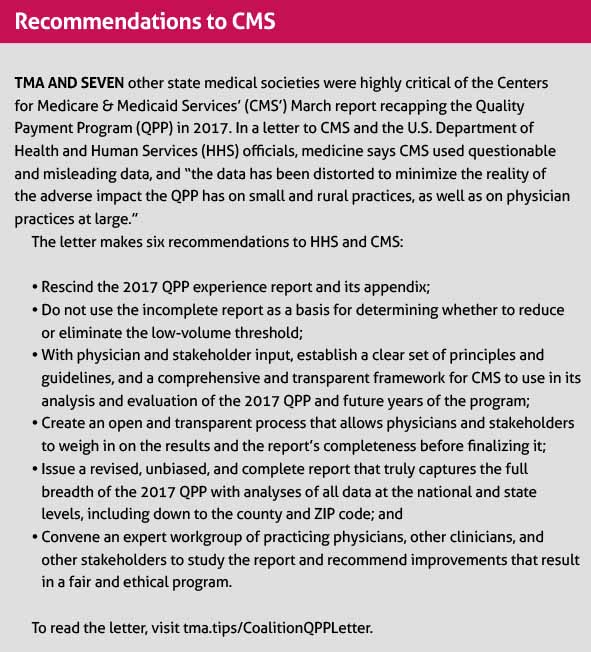
Ultimately, the letter says CMS should not act alone in the “selection of data, analysis of performance, and evaluation of the QPP experience.” Instead, to improve the integrity of the report, practicing physicians actively participating in QPP and other stakeholders with expertise in the program should contribute to it, TMA says. The letter concludes with six recommendations for CMS, beginning with rescinding the report altogether. (See “Recommendations to CMS,” page 36.)
Dr. Fleeger says he’s not convinced that the QPP differentiates between high-quality and low-quality physicians, as it’s supposed to do. “Mainly,” he said, “it’s differentiating who’s able to perform the bureaucratic paperwork necessary to receive the points in order to qualify as participating. And yet we still have 1,830 physicians in Texas who will be penalized.”
TMA, he adds, “has an obligation to try to fight federal and state and private-payer bureaucracies that burden our physicians. And if we can’t get those burdens relieved, then we have an obligation to try and help our members comply.
“That’s what TMA does: Try to help our physicians. But as it stands now, it seems like the system disadvantages those who can least tolerate having the penalty.”
Tex Med. 2019;115(6):32-37
June 2019 Texas Medicine Contents
Texas Medicine Main Page