
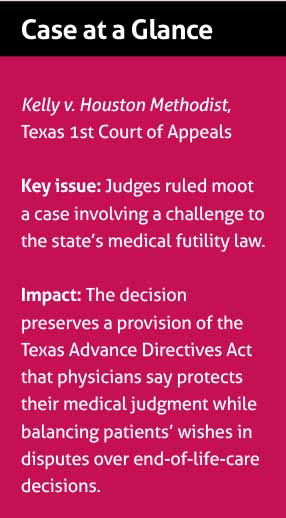
For the second time in less than two years, a Texas court has thrown out a challenge to what the Texas Medical Association believes is an essential part of the state’s advance directives law.
The 1st Court of Appeals ruled in March that the case Evelyn Kelly filed on behalf of her late son, David Christopher Dunn, was moot because her son’s rights were not violated by the hospital’s use of the Texas’ medical futility law. Following Mr. Dunn’s death in December 2015, Ms. Kelly mounted a challenge to the law, which allows physicians to initiate an ethics-committee review of a patient’s case if the family disagrees with the doctors’ medical judgment to withhold or withdraw life-sustaining treatment.
Twice now, TMA, the Texas Alliance for Patient Access (TAPA), and several other organizations have weighed in on the case with a joint friend-of-the-court brief supporting the law. Both times, courts have effectively upheld the ethics-committee process that physicians view as crucial to protecting their medical judgment in end-of-life care decisions.
TAPA and TMA said in their brief that the advance directives law, passed in 1999, “respects the patient’s wishes and leaves room for good-faith differences of medical opinion.”
Fort Worth internal medicine physician Stuart Pickell, MD, says the medical futility law, while not perfect, is one of Texas’ most important statutes.
“Before ethics committees, it was up to the doctor. The doctor would just decide,” Dr. Pickell said. “So ethics committees have actually liberalized that quite a bit, in the sense of providing more time and space for a controversial decision to be discussed … and assessed.”
How the law works
If a physician believes giving a patient life-sustaining treatment would exacerbate or extend that person’s suffering, but the patient or a patient’s representative wants it done anyway, the Texas Advance Directives Act provides an avenue to resolve that dispute and protect physicians from liability.
Under the medical futility part of the law, the physician can take the patient’s case to the hospital’s ethics committee. If the ethics committee agrees with the physician that the treatment isn’t medically appropriate, the hospital must make a reasonable effort to transfer the patient to another facility within 10 days. After making that transfer attempt, the physician is immune from both civil and criminal liability for either withholding or stopping treatment.
Most hospital ethics committees contain broad representation from physicians, other health care professionals, social workers, chaplains, and members of the hospital’s administrative and legal teams, says Dr. Pickell, who has worked with several such committees.
“If there’s a problem [with ethics committees], it’s that they’re not involved early enough. A lot of times, they are consulted after the problem has escalated. It’s always easier to put out a forest fire when it’s still a campfire,” Dr. Pickell said.
A difficult decision
According to court filings, Mr. Dunn was admitted to Houston Methodist Hospital in October 2015 to treat an “unidentified mass on his pancreas which caused damage to other organs.” He was diagnosed with end-stage liver disease, acute renal failure, acute respiratory failure, and other illnesses. The hospital began life-sustaining treatment, but his treating physicians soon concluded the care was making him suffer. Mr. Dunn’s father agreed with their recommendation to withdraw that treatment; his mother, Ms. Kelly, did not, court records show.
In November 2015, the hospital’s ethics committee initiated a review in which it agreed with the care team. But attorneys representing the patient initiated legal action, and the hospital agreed to a temporary restraining order and kept him on life-sustaining treatment. Mr. Dunn stayed on that treatment until his death on Dec. 23, 2015. After his death, Ms. Kelly released a statement thanking Methodist for continuing the treatment and vowed “to continue to fight against this horrible law.”
She did so with a February 2016 lawsuit, which alleged a violation of her and her son’s due process rights. Among other claims, the suit said the hospital “prematurely applied the procedures” of the medical futility law, and that the law “allows doctors and hospitals the absolute authority and unfettered discretion” to terminate any patient’s life-sustaining treatment, even if an advance directive is in place.
In September 2017, a Harris County district judge ruled the legislature, not the court, is the proper place to apply any potential fix to the law. Ms. Kelly appealed that decision.
No rights violated
In March, TMA – just as it had done prior to the 2017 court decision – joined a friend-of-the-court brief with TAPA, the Texas Hospital Association, the Texas Catholic Conference of Bishops, and others.
The brief argued that “the forced provision of medically inappropriate treatment threatens the proper and ethical practice of medicine.” Texas’ law on end-of-life care and the immunity it grants in exchange for properly following the ethics committee procedure represent good law, the brief says. Physicians invoke that process “because they believe that medical intervention will no longer benefit the patient but instead will only inflict suffering.”
Just weeks after medicine filed its brief, appellate judges upheld the trial court’s decision. Justice Julie Countiss wrote that “no action inconsistent with Dunn’s alleged desires regarding his medical treatment was ever taken and he was not actually deprived of any constitutionally-protected right” when Methodist invoked the law. There is “no right to due process if there has not been a deprivation of a constitutionally-protected interest,” the ruling says.
An attorney for Methodist declined comment for this story. An attorney for Ms. Kelly did not return a phone call from Texas Medicine.
Tex Med. 2019;115(6):17-18
June 2019
Texas Medicine Contents Texas Medicine Main Page