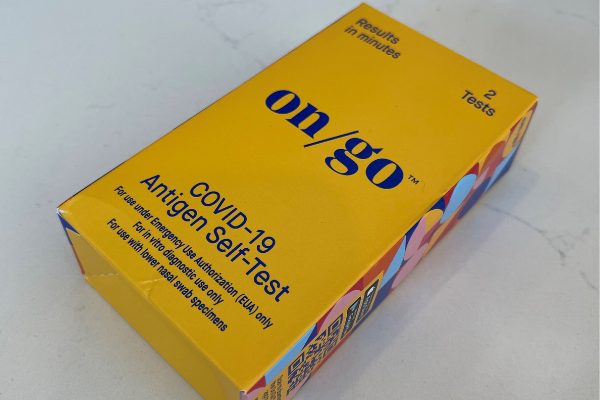
The Biden-Harris administration is requiring insurers and group health plans to cover the cost of over-the-counter, at-home COVID-19 tests beginning this Saturday, Jan. 15, the U.S. Department of Health and Human Services (HHS) announced.
While the Texas Medical Association welcomes the administration’s plan, it remains concerned about the limited availability of the at-home tests, says Rodney Young, MD, chair of TMA’s Council on Socioeconomics.
“Removing the cost barrier and expanding access to these tests are important steps toward helping us contain the virus, provided the tests are widely available and that we follow the [Centers for Disease Control and Prevention’s] quarantine and isolation guidance appropriately in response to the results,” Dr. Young said.
The increased access to free home testing is part of the administration’s actions last month to combat the rapid spread of the omicron variant of the virus.
“Insurance companies and health plans are required to cover eight free over-the-counter at-home tests per covered individual per month. That means a family of four, all on the same plan, would be able to get up to 32 of these tests covered by their health plan per month,” the agency said. “There is no limit on the number of tests, including at-home tests, that are covered if ordered or administered by a health care provider following an individualized clinical assessment, including for those who may need them due to underlying medical conditions.”
Also part of the requirement are incentives for insurers and group plans to set up programs allowing people “to get the over-the-counter tests directly through preferred pharmacies, retailers, or other entities with no out-of-pocket costs,” HHS said. “Insurers and plans would cover the costs up front, eliminating the need for consumers to submit a claim for reimbursement. When plans and insurers make tests available for upfront coverage through preferred pharmacies or retailers, they are still required to reimburse tests purchased by consumers outside of that network, at a rate of up to $12 per individual test (or the cost of the test, if less than $12).”
State Medicaid and Children’s Health Insurance programs are already required to cover at-home COVID-19 tests without patient cost-sharing.
More information on obtaining the at-home tests is available on the Centers for Medicare & Medicaid Services website.